Session Information
Date: Sunday, November 7, 2021
Title: Measures & Measurement of Healthcare Quality Poster (0623–0659)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Cardio-metabolic abnormalities are common in patients with inflammatory arthritis (IA) but tend to be under-recognized and under-treated. We aimed to compare the prevalence and risk factors for cardio-metabolic abnormalities between patients with rheumatoid arthritis (RA), psoriatic arthritis (PsA) and ankylosing spondylitis (AS).
Methods: Consecutive patients enrolled in the University of Toronto Cardio-Rheumatology Network from 2017 to 2020 were analyzed. This is a primary prevention program that uses structured clinical, laboratory and multimodal imaging to diagnose and treat cardiovascular disease (CVD). Patients with a rheumatologist-confirmed diagnosis of RA, PsA or AS and no known CVD were evaluated. Information about IA diagnosis, medications and comorbidities was recorded. Each patient was evaluated by a cardiologist focusing on CVD risk assessment. We evaluated the prevalence of previously recorded and newly recognized cardio-metabolic risk factors including hypertension, dyslipidemia, obesity and diabetes. The prevalence of these abnormalities was compared between IA diagnoses. Regression models were used to assess the association between diagnosis and cardio-metabolic abnormalities after adjusting for demographics, smoking, BMI, measures of disease activity and medications.
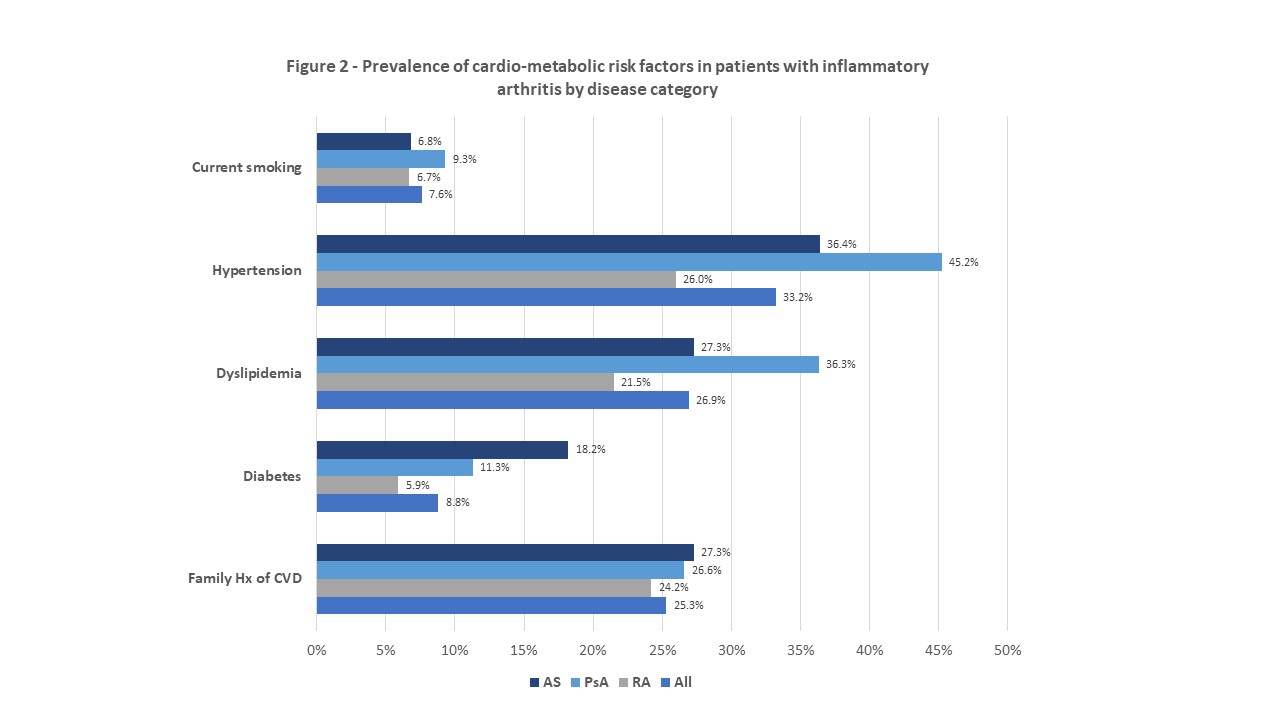
Results: A total of 376 patients (219 RA, 124 PsA, 33 AS) were assessed (mean age 59±10.4 years, 69.7% female). Hypertension was reported in 33.2%, dyslipidemia in 26.8%, diabetes mellitus in 8.8% and overweight/obesity in 68.7%. Newly diagnosed dyslipidemia (elevated total cholesterol), elevated blood pressure and diabetes occurred in 40.3%, 14.8% and 1.5% of all patients (Figure 1). A total of 32% patients required a change or initiation of medications for their cardio-metabolic abnormalities (21.7% lipid-lowering therapy, 13.4% aspirin, 10.9% anti-hypertension therapy). Patients with PsA had the highest prevalence of cardio-metabolic abnormalities including dyslipidemia, obesity and hypertension (Figure 2). Having hypertension (prior or new diagnosis), elevated levels of triglycerides, non-HDL cholesterol, total cholesterol and BMI were associated with PsA vs. RA after adjusting for potential confounders (Figure 3). No significant association was found between cardio-metabolic abnormalities and AS vs. PsA or RA.
Conclusion: Dedicated cardio-rheumatology clinics have improved CVD screening and management in an IA population. The burden of cardio-metabolic abnormalities is elevated in PsA and suggests that tailored strategies to reduce adverse CVD events are particularly needed in this subgroup.
To cite this abstract in AMA style:
Eder L, Akhtari S, Jerome D, Udell J, Lawler P, Harvey P, Kuriya B. Prevalence and Risk Factors for Cardio-metabolic Abnormalities in Patients with Inflammatory Arthritis Attending Cardio-rheumatology Primary Prevention Clinics [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/prevalence-and-risk-factors-for-cardio-metabolic-abnormalities-in-patients-with-inflammatory-arthritis-attending-cardio-rheumatology-primary-prevention-clinics/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-risk-factors-for-cardio-metabolic-abnormalities-in-patients-with-inflammatory-arthritis-attending-cardio-rheumatology-primary-prevention-clinics/