Session Information
Date: Sunday, November 7, 2021
Title: Measures & Measurement of Healthcare Quality Poster (0623–0659)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Prior studies have described increased incidence of cervical dysplasia and cervical cancer in women with systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA), suggesting that these populations are at higher risk due to their disease state, their immunosuppressive medications, or both. The current US Preventive Services Task Force (USPSTF) guidelines recommend cervical cancer screening in women ages 21-65 years at intervals of 3-5 years based on age and HPV co-testing. Our aim was to assess the proportion of women with SLE and RA with documented cervical cancer screening per these guidelines.
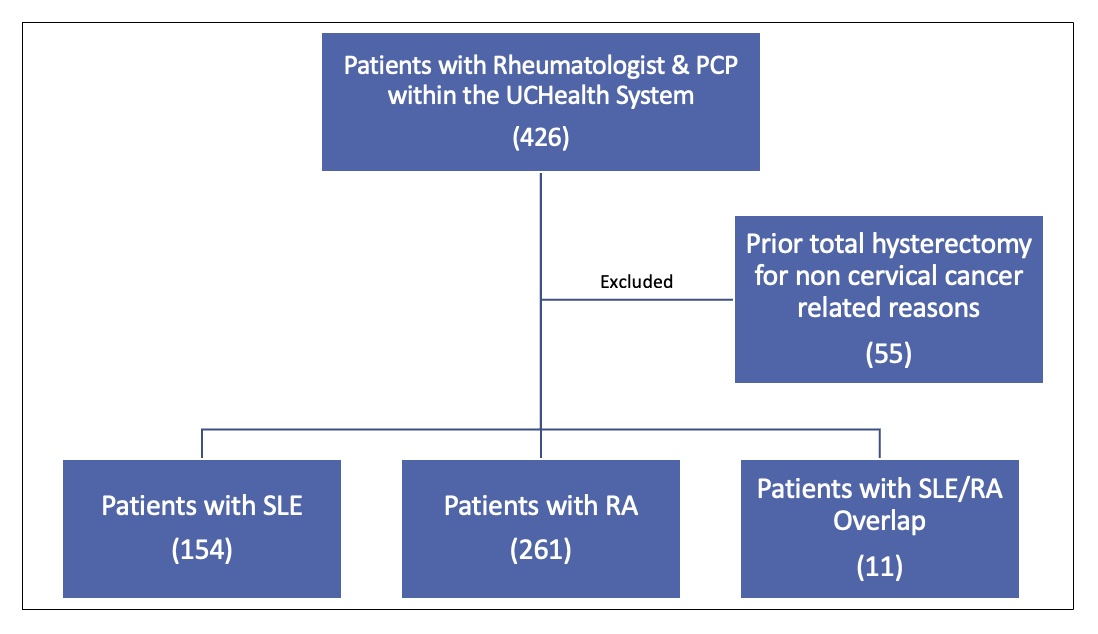
Methods: This was a single-system retrospective chart review of women ages 21-65 years with SLE and RA. Included patients had a rheumatologist and primary care provider (PCP) within our university health system. For each patient, we documented the date and result of last Pap smear. We calculated each patient’s age at last Pap smear, and for patients ages 21-29, we assessed for Pap smear within the last 3 years. For thoses ages 30-65, we assessed for Pap smear within 3 years or within 5 years with HPV cotesting. We excluded those with hysterectomy for non-cervical cancer reasons, and analyzed the proportion of remaining patients with abnormal cervical cancer screening results.
Results: Of the 371 patients included in the final analysis (Figure 1), 285 (76.8%) had age-appropriate cervical cancer screening documented in the medical record per USPSTF guidelines, compared to 81% of all women nationally. 50 of the 371 patients (13%) had no prior cervical cancer screening data available in the chart. Of all 371 patients, last documented Pap smear was abnormal in 28 (7.5%). Of those patients, 18 had a positive HPV test. 3 rheumatology providers had ever documented the status of last Pap smear, and none documented counseling on cervical cancer screening.
Conclusion: Our results indicate that PCPs within our health system screen for cervical cancer in patients with SLE and RA at rates similar to the national average for all women. We acknowledge that our data may be underestimating the true number for our patients, as 13% had no prior documented Pap smear in the system. The current national average for cervical cancer screening is suboptimal, but it is even more unacceptable in patients with SLE and RA given their increased risk for cervical dysplasia. One barrier may be insufficient education about the association between these disease states and cervical cancer risk. We propose that there is an underutilized role for rheumatologists in educating patients and their PCPs about risk mitigation.
To cite this abstract in AMA style:
Skorupa T, Khatter S, Freifeld A, Weinstein E. Assessing the Rates of Cervical Cancer Screening in Women with Systemic Lupus Erythematosus and Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/assessing-the-rates-of-cervical-cancer-screening-in-women-with-systemic-lupus-erythematosus-and-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessing-the-rates-of-cervical-cancer-screening-in-women-with-systemic-lupus-erythematosus-and-rheumatoid-arthritis/