Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Despite treatment advances, ANCA-associated vasculitis (AAV) remains associated with excess morbidity and mortality. Interstitial lung disease (ILD) is an increasingly recognized manifestation of AAV but its prevalence, characteristics, and outcomes remain poorly defined. Additionally, most studies of AAV-ILD have been performed in AAV cohorts assembled in Asia where MPO-ANCA+ disease is highly prevalent. We sought to characterize factors associated with AAV-ILD and mortality in AAV-ILD in a large North-American-based AAV cohort.
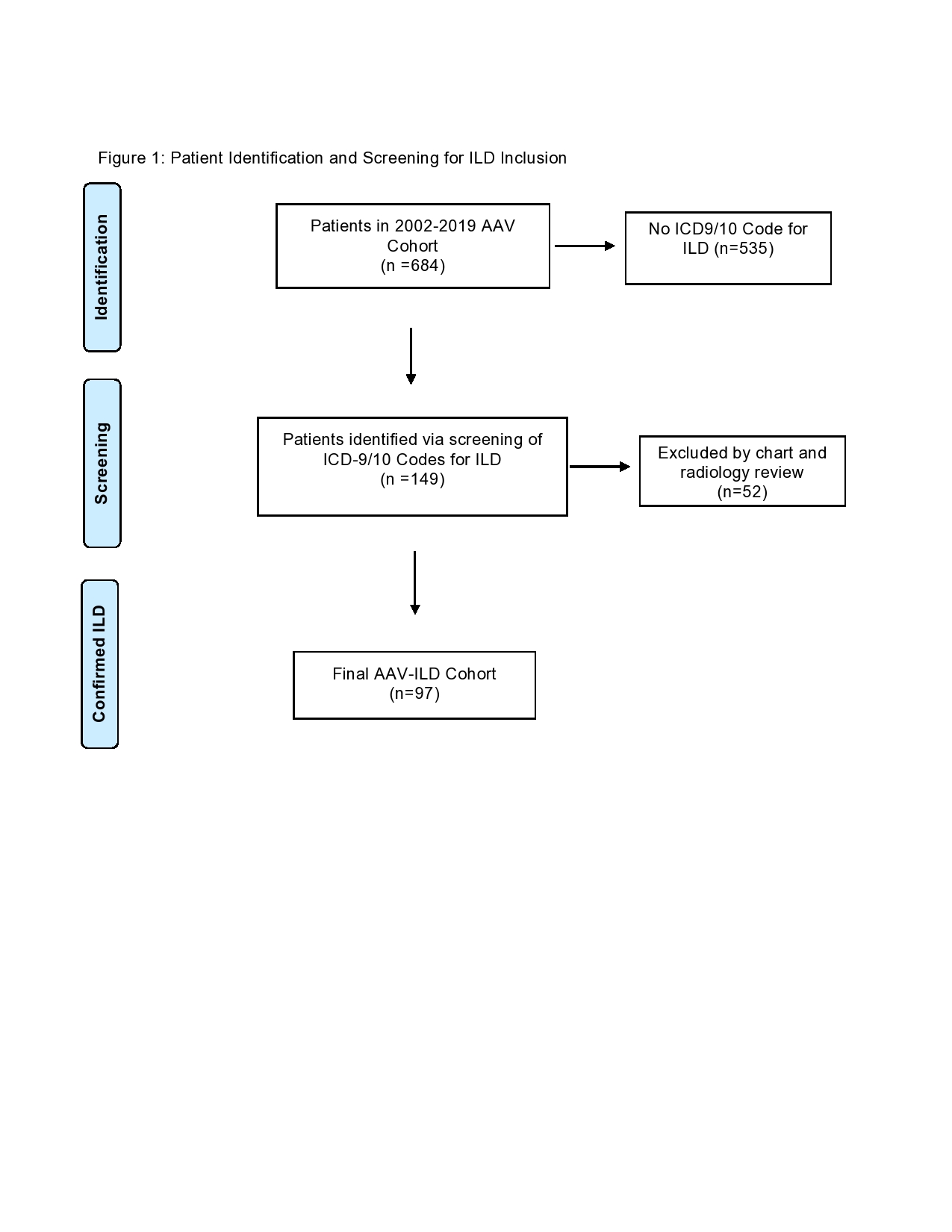
Methods: AAV-ILD cases were identified by screening a consecutive inception PR3- or MPO-ANCA+ AAV multi-center cohort assembled between 2002 and 2019 for ICD-9/10 codes relevant to the diagnosis of ILD. Each case identified by this screen then underwent a manual review of the electronic health record (EHR) and available chest imaging. Two board-certified radiologists reviewed all available computer tomography (CT) scans of the chest for each patient to assess for interstitial lung disease and classify the type of ILD (UIP vs non-UIP). Patients with uncertain radiographic features were considered to not have ILD. Demographics, AAV disease features, results of pulmonary function tests, and comorbidities were extracted from the EHR. The baseline Birmingham Vasculitis Activity Score/Wegener’s Granulomatosis (BVAS/WG) was determined for each patient. All-cause mortality was assessed by linkage to the National Death Index. Univariate analyses were used to assess the association of demographic- and disease-specific factors with AAV-ILD. Unadjusted and adjusted Cox proportional hazard models with age as the time scale were used to assess the association of AAV-ILD with death among patients with AAV.
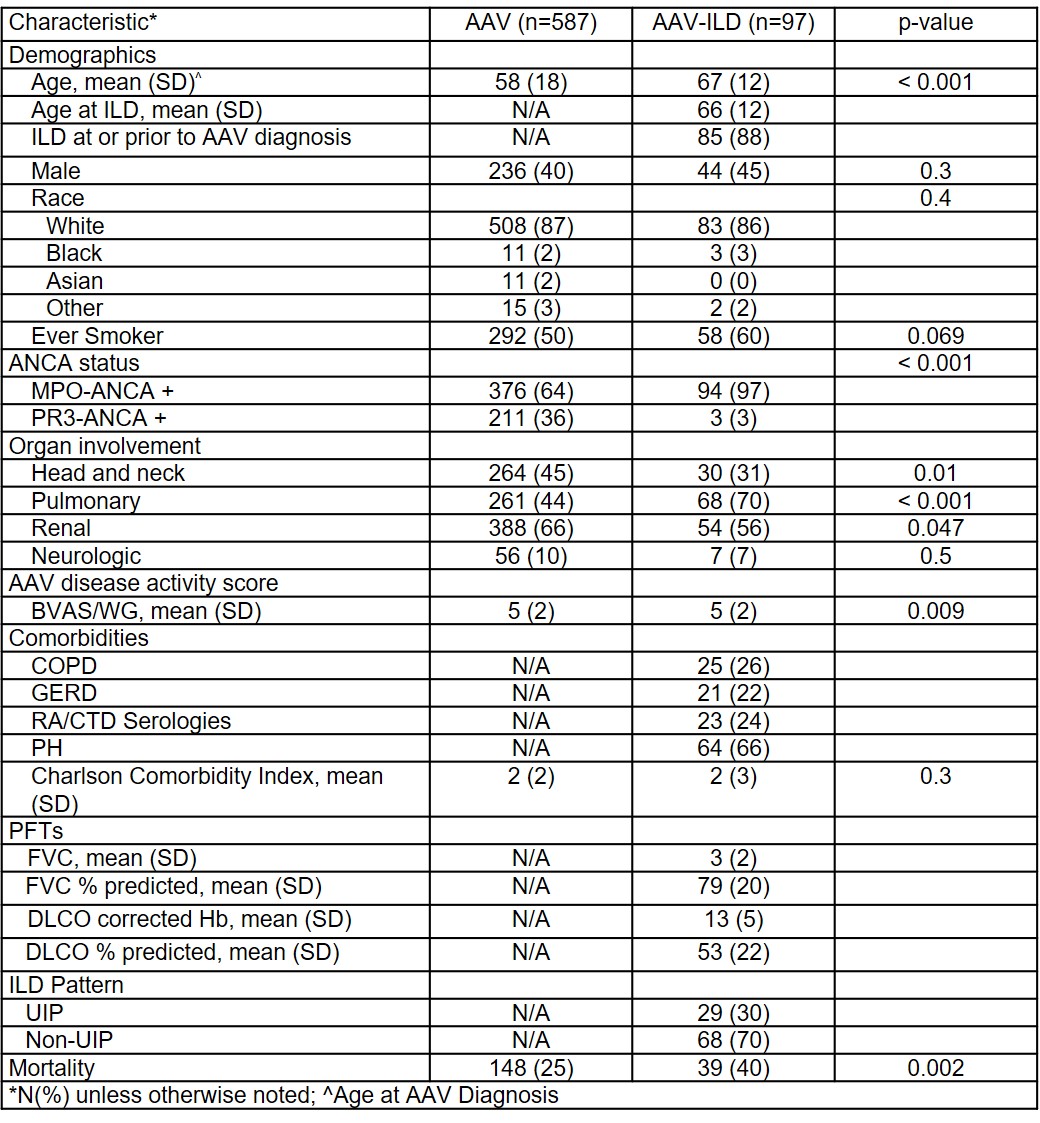
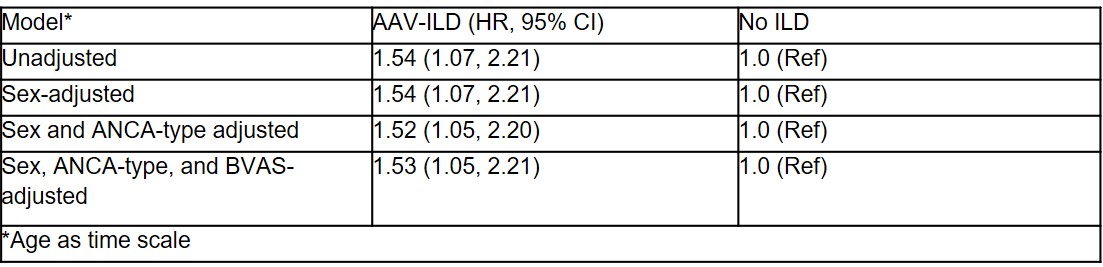
Results: Of 698 patients from the cohort, 14 were excluded because of insufficient records and 684 were screened (Figure 1). Of those screened, 97 (14.2%) had AAV-ILD. Patients with AAV-ILD were older (67±12yrs vs 58±18yrs, p< 0.001) than those with AAV-non-ILD; sex distribution was similar (55% vs 60% female, p=0.7) (Table 1). Compared to AAV-non-ILD, AAV-ILD patients were more often MPO-ANCA+ (97% vs. 64%, p< 0.001) and less often had head and neck involvement (31% vs 45%, p=0.01). The diagnosis of ILD preceded or occurred concurrently with the diagnosis of AAV in 85 (88%) patients. The ILD pattern was classified as UIP in 29 (30%) patients with AAV-ILD. The mean (SD) FVC % predicted among AAV-ILD patients was 79±20% and adjusted DLCO % predicted was 53±22% (Table 1). AAV-ILD was associated with a 53% higher risk of death than AAV-non-ILD in analyses adjusted for age, sex, baseline BVAS/WG, and ANCA type (HR=1.53, 95% CI 1.05, 2.21) (Table 2).
Conclusion: In a large North American cohort of AAV patients, we estimated the prevalence of AAV-ILD as 14% and observed strong associations with MPO-ANCA positive disease. In the vast majority of cases, AAV-ILD was present prior to or at the time of AAV diagnosis, highlighting that it is a feature that may precede other manifestations of AAV. Compared with AAV patients without ILD, those with ILD have a higher risk of all-cause mortality. Additional studies are needed to understand the response of ILD in AAV to conventional AAV treatment regimens.
To cite this abstract in AMA style:
Doliner B, Rodriguez K, Montesi S, Fu X, Sharma A, Wallace Z. Interstitial Lung Disease in ANCA-Associated Vasculitis: Associated Factors and Outcomes [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/interstitial-lung-disease-in-anca-associated-vasculitis-associated-factors-and-outcomes/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/interstitial-lung-disease-in-anca-associated-vasculitis-associated-factors-and-outcomes/