Session Information
Date: Saturday, November 6, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Diagnosis (0323–0356)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Lupus nephritis (LN) is a leading cause of morbidity and mortality in systemic lupus erythematosus (SLE) patients. While LN pathogenesis has yet to be fully elucidated, T cells have been strongly implicated in mechanisms of disease. CD6 is a co-stimulatory receptor on T cells, that binds to activated leukocyte cell adhesion molecule (ALCAM), a ligand expressed on antigen presenting cells and epithelial and endothelial tissues. The CD6-ALCAM pathway plays an integral role in modulating T cell activation and trafficking and is central to immune-mediated inflammation. Previously, we reported that soluble urine ALCAM is a potential biomarker of disease in LN. Here, we evaluated the correlation of serum and urine ALCAM and CD6 with disease activity over time.
Methods: Patient samples were acquired through the Accelerating Medicines Partnership (AMP), a public-private partnership to accelerate development of therapeutics for diseases such as LN. Serum and urine samples were obtained from patients with biopsy proven LN (n=345) and living kidney donor controls (n=68). Follow-up longitudinal sampling (3, 6, and 12 months) was available for 143 LN patients. ALCAM levels were quantified by ELISA, while CD6 levels were quantified by an electrochemiluminescent assay. Levels were analyzed cross-sectionally (first visit) and longitudinally against disease measures that included proteinuria, SLEDAI, the renal components of the SLEDAI score (R-SLEDAI), ISN-RPS histological class of the lesion, serological parameters, and patient characteristics.
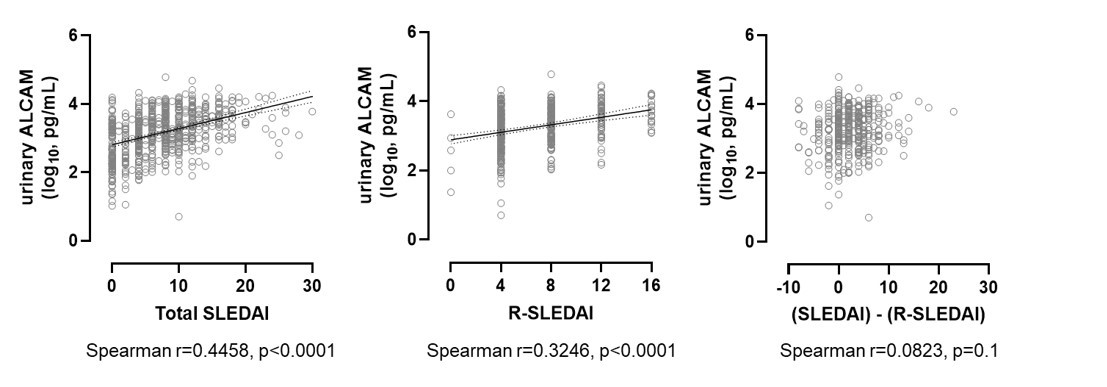
Results: Consistent with our previous findings, cross-sectional analysis showed that urinary ALCAM was significantly elevated in LN patients (mean 4333.5 pg/mL, 95% CI [3614.0, 5053.0]) compared to control subjects (mean 214.4 pg/mL, 95% CI [152.9, 276.0]) (p< 0.001), but that there were no differences in serum ALCAM levels. Urinary ALCAM levels significantly correlated with SLEDAI and R-SLEDAI scores (but did not correlate to the non-renal portion of SLEDAI (SLEDAI – R-SLEDAI) (Figure 1), suggesting that ALCAM level is associated with the renal activity. This was supported by near-significant correlations with C3 (p=0.07) and C4 levels (p=0.05). Serum and urine levels of CD6 were similar between cases and control subjects and did not change with disease activity, suggesting that the differences observed in urinary ALCAM levels are not due to hemodynamic changes or non-specific loss of glomerular permeability. In patients followed with longitudinal sampling, urinary ALCAM reflected changes in SLEDAI and R-SLEDAI. Furthermore, in preliminary analysis of a subset of patients who exhibited significant changes in R-SLEDAI across visits, intra-patient comparison of the respective timepoints reflected concomitant significant changes in urinary ALCAM levels (Figure 2).
Conclusion: Here, we expand upon previous studies and provide additional support in a large multi-center cohort, by showing that urinary ALCAM levels are elevated in SLE patients with active LN and decline with clinical improvement. Studies in progress are evaluating the implications of these findings in predicting therapeutic responses in LN, as well as longer term disease outcomes and prognosis.
To cite this abstract in AMA style:
Chu D, Schwartz N, Ampudia J, Guthridge J, James J, Buyon J, Connelly S, Fung M, Ng C, Mohan C, Putterman C. Soluble Urine ALCAM Reflects Renal Disease Activity in Lupus Nephritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/soluble-urine-alcam-reflects-renal-disease-activity-in-lupus-nephritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/soluble-urine-alcam-reflects-renal-disease-activity-in-lupus-nephritis/