Session Information
Session Type: Abstract Session
Session Time: 3:00PM-3:50PM
Background/Purpose: Rheumatoid arthritis (RA) is a risk factor for osteoporosis and fractures yet the disease specific contributions to osteoporotic fractures (OFX) are not well understood. Chronic inflammation stimulates bone loss leading to low bone mineral density and also has negative effects on muscle mass and function, further amplifying the risk of falls and fractures. Our goal was to study whether RA disease activity, and its subcomponents, were independently associated with incident OFX.
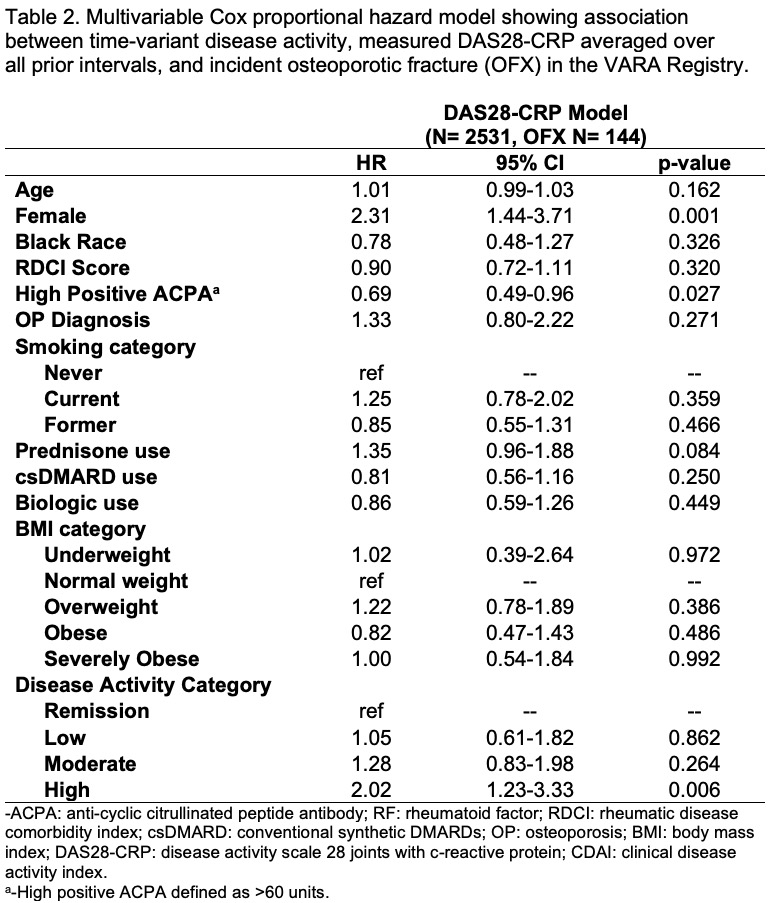
Methods: We used the multicenter Veterans Affairs RA (VARA) registry, including participants with at least 1 DAS28-CRP measure in the analysis. Extremity, spine, and hip OFX were identified by ICD9/10 codes from inpatient and outpatient encounters and were confirmed by chart review. Cox proportional hazard models were used to assess the association between time-variant disease activity (averaged over all prior intervals) and incident OFX controlling for baseline sex, race, high ACPA ( >60 units), rheumatic disease comorbidity index, osteoporosis status and time-variant age, BMI, smoking, prednisone use, conventional synthetic DMARDs (csDMARDs) and biologic use. Baseline osteoporosis diagnosis was defined by ICD9/10 code or prior fracture. We used DAS28-CRP in our primary analysis but also considered clinical disease activity index (CDAI) and individual RA disease activity components (Tender Joint Count (TJC), Swollen Joint Count (SJC), Patient Global Assessment (PatGA), Provider Global Assessment (PrGA), and CRP) in secondary analyses.
Results: Among 2,531 Veterans followed for 10,661 patient-years (including 25,694 unique observations), 145 incident OFX were identified at a rate of 1.4 per 100 person-years. Veterans were on average 71.2±10.5 years old, 11% were female, 79% were seropositive, and 10% had a diagnosis of osteoporosis at baseline (Table 1). High disease activity by average DAS28-CRP was associated with a significantly greater risk of incident OFX [HR 2.02 (1.22-3.33), p=0.006] (Table 2) compared to those in remission. In secondary analyses, high RA disease activity by CDAI was also associated with an increased risk of OFX [HR 3.56 (1.24-10.17), p=0.018]. All of the individual disease activity components were associated with a greater risk of OFX except TJC (Table 3). Female sex and high ACPA were significantly associated with higher and lower risks for OFX [HR 2.31 (1.44-3.71) and HR 0.69 (0.49-0.96), p< 0.05].
Conclusion: High RA disease activity is associated with twice the risk of OFX compared to those whose disease is in remission. All of the individual disease activity components were associated with a greater risk of OFX except TJC. The degree of control of RA disease activity may represent a modifiable risk factor for OFX. Studies evaluating the specific mechanisms that drive the association between RA disease activity and OFX are needed to inform interventions focused on preventing this outcome.
To cite this abstract in AMA style:
Wysham K, Mikuls T, England B, Shoback D, Katz P, Garcia J, Sauer B, Wallace B, Richards J, Monach P, Cannon G, Baker J. High Disease Activity Is Associated with Incident Osteoporotic Fractures Among Veterans with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/high-disease-activity-is-associated-with-incident-osteoporotic-fractures-among-veterans-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/high-disease-activity-is-associated-with-incident-osteoporotic-fractures-among-veterans-with-rheumatoid-arthritis/