Session Information
Session Type: Abstract Session
Session Time: 12:00PM-12:50PM
Background/Purpose: Previous studies have shown that sociodemographic factors are associated with quality of care. Using the Rheumatology Informatics System for Effectiveness (RISE) registry, we assessed whether the area deprivation index (ADI) and/or race/ethnicity was associated with provider performance on quality measures among patients with rheumatoid arthritis (RA).
Methods: We analyzed data collected on all patients with a diagnosis of RA who had at least one clinic visit between January 2015 and December 2017. We examined performance on disease activity assessment, functional status assessment, tuberculosis (TB) screening prior biologic start and blood pressure (BP) control. Using mixed-effects regression, we assessed the effect of area deprivation (as measured by the ADI, above or below the median percentile, where higher scores reflect more deprivation) and race/ethnicity on measure performance and on change in performance over time. Since practice characteristics could mediate this effect, we controlled for practice type, number of providers, region, and eHR software. Analyses accounted for clustering by practice and by patient.
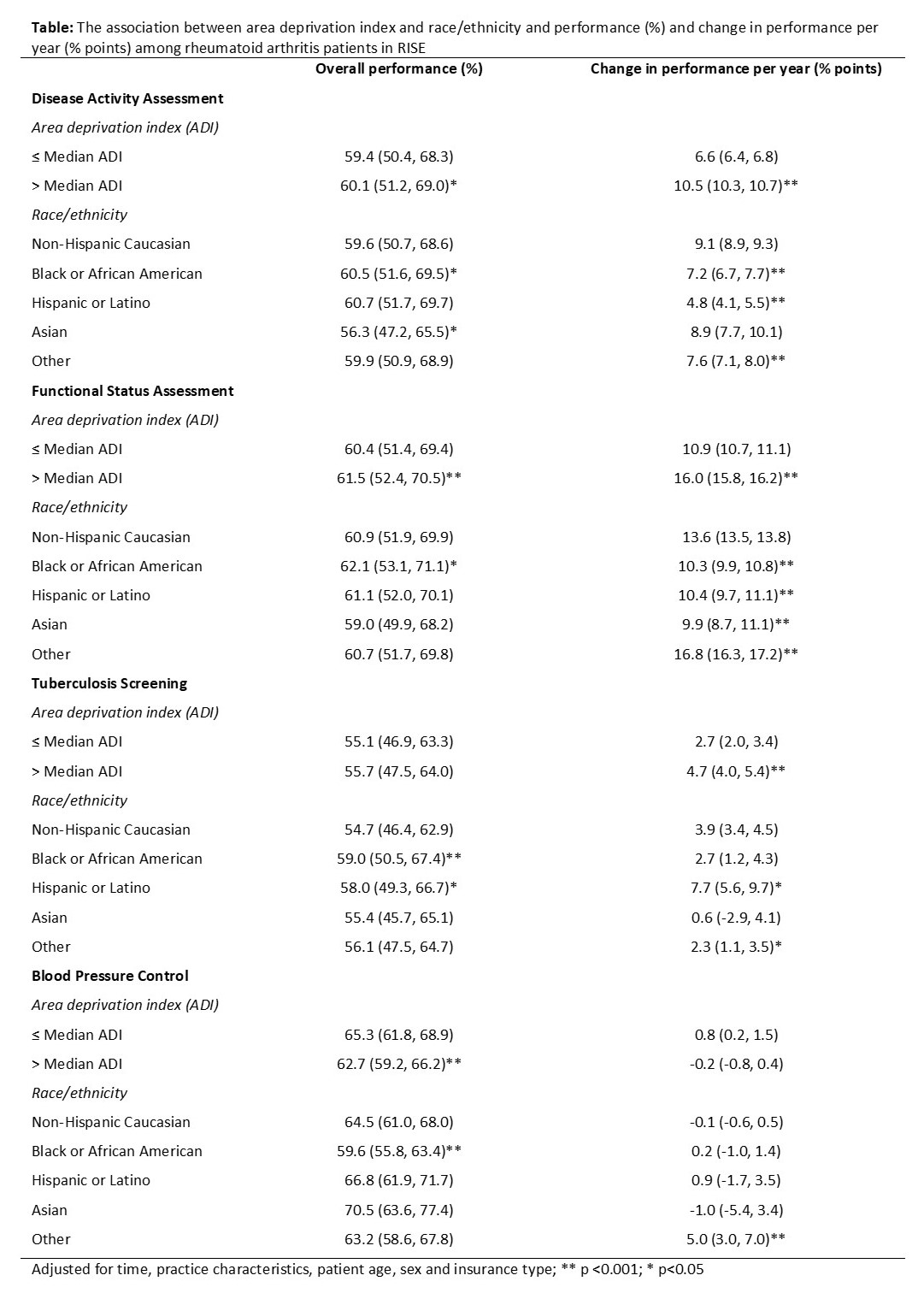
Results: Data from 58,432 patients from 54 practices was examined. Mean age was 63±14 years, 77% were female, and 69% were Caucasian. Over time, there were significant improvements in performance on functional status assessment (+13.5% per year) and disease activity assessment (+8.8%), smaller improvements in performance on TB screening (+2.9%) and no improvements in performance on BP control. Performance on disease activity assessment and functional status assessment was comparable across all subgroups (Table). Both measures improved faster over time among patients with higher ADI, but improvements were slower among African Americans and Hispanics than Caucasians. Performance on TB screening was higher among African Americans (59.0%) and Hispanics (58.0%) than Caucasians (54.7%) and improved faster over time among Hispanics (+7.7% points per year) than Caucasians (3.9%, p< 0.05) and among patients with higher ADI (+4.7%) than those with lower ADI (+2.7%, p< 0.001). Performance on BP control was lower among African Americans (59.6%) and patients with higher ADI (62.7%) than Caucasians (64.5%, p< 0.001) and patients with lower ADI (65.3%, p< 0.001), respectively.
Conclusion: Although performance on quality measures is improving overall, we found important differences across sociodemographic groups. Non-Caucasians and those with lower socioeconomic status (SES) had less improvement compared to Caucasians and those with higher SES. TB screening seems to be improving more among higher risk groups. Consistent with studies in the general medical literature, BP control was lowest among African Americans. To address health disparities, future quality improvement initiatives should target patient groups with persistent gaps in quality of care.
To cite this abstract in AMA style:
Izadi Z, Schmajuk G, Yazdany J. Variation in Quality of Care Among Patient Sociodemographic Groups in RISE Practices [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/variation-in-quality-of-care-among-patient-sociodemographic-groups-in-rise-practices/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/variation-in-quality-of-care-among-patient-sociodemographic-groups-in-rise-practices/