Session Information
Date: Monday, November 9, 2020
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Lack of sensitivity or specificity of symptoms may induce uncertainty in diagnosis and classification of AS/axSpA. We investigated if balanced sensitivity and specificity of tools from the patient’s clinical history may help better define the ‘Gestalt’ of AS/axSpA
Methods: In 1985 members of the Swiss AS Patient Society who had been diagnosed as having AS by their own physicians, as well as their first degree relatives (FDRs) were invited to participate in the current study. After obtaining ethical approval and informed consent, 1178 subjects, 363 of them probands, formed our study cohort; they completed questionnaires on disease manifestations, underwent rheumatological examination of axial and peripheral joints, and provided blood samples for genetic studies, including HLA-B27. Probands also provided a recent pelvic radiograph to document presence of sacroiliitis. If their pelvic radiograph was not available, it was performed on-site. Relatives aged ≥18 years underwent pelvic radiography, unless pregnant. Pelvic radiographs were available for 360 probands and 713 relatives. Radiographs were blindly assessed twice by each of 4 readers. The assessment could only be performed once for 164 (46%) of the 360 radiographs of the probands (available only for a few hours). The sacroiliitis score for each sacroiliac (SI) joint ranged from 0 (normal) to 4 (ankylosis). Scores were added and then divided by the number of assessments. Scores below bilateral grade 2.0 or grade 3.0 unilaterally were considered not meeting New York radiographic criteria (NYRC).
In 2018 the ethical committee of the Swiss Kanton of Bern approved the follow-up study. Many Swiss city and village administrations provided current addresses of former participants. By December 2019, 123 probands and 39 FDRs had died, and 462 consenting participants completed a 157 item postal disease related questionnaire dealing with symptoms at lumbar and gluteal region, thoracic spine, and front part of the chest.
The gold standard for sensitivity was AS patients meeting NYRC for AS. The gold standard for specificity was the HLA-B27(-) relatives of HLA-B27(+) probands, as this group have a near zero chance of developing axSpA. Statistical analysis was performed by chi-square test.
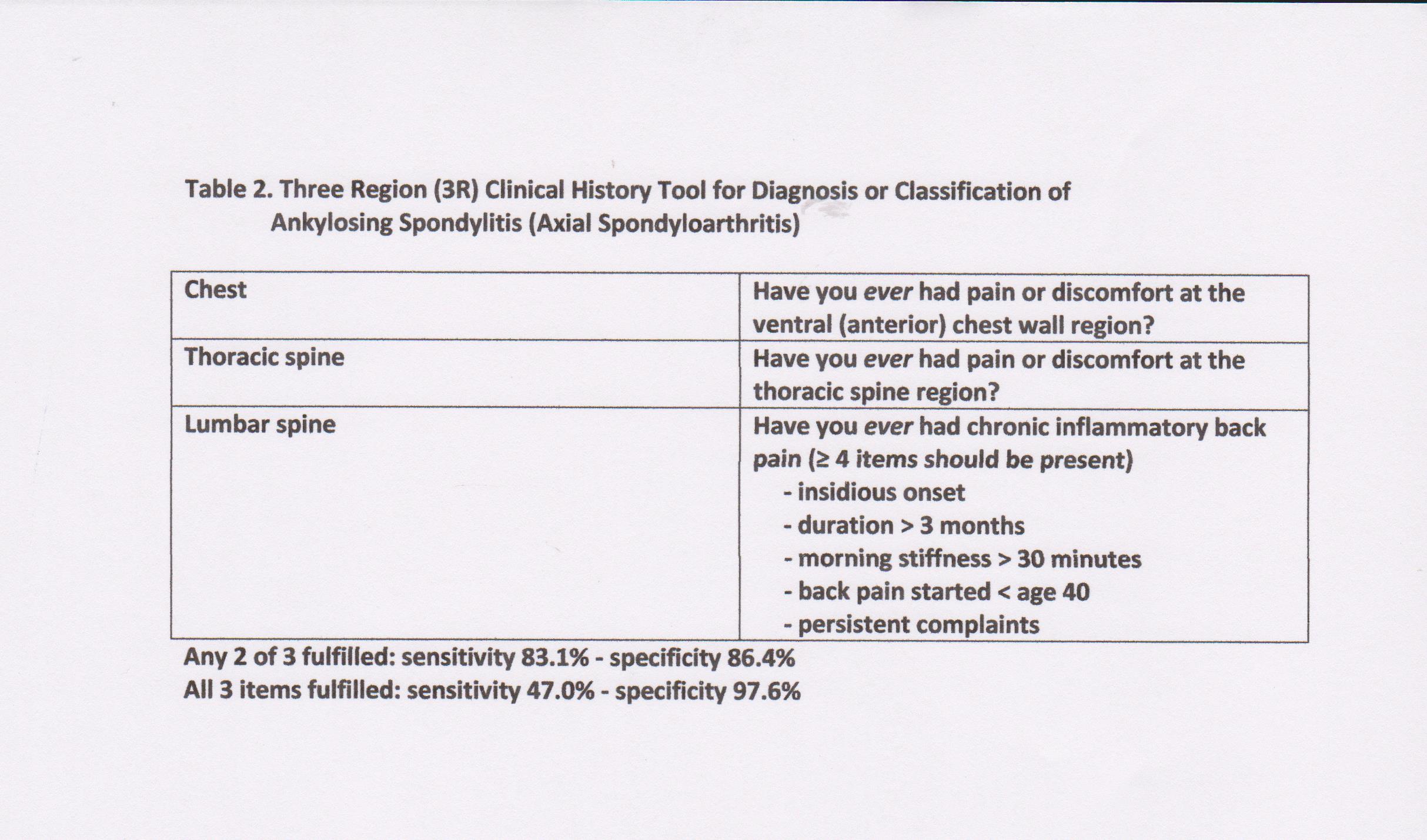
Results: Sensitivity was assessed in 88 (85 of them HLA-B27(+)) AS patients (mean age 72.1 ± 7.5 years) meeting the NYRC, and specificity in the group of 130 HLA-B27(-) relatives (mean age 62.8 ± 9.2 years). Table 1 shows by anatomical region the questionnaire items that have sensitivity or specificity > 70% and likelihood ratio (LR) values ≥ 2. None of the criteria individually demonstrate sensitivity and specificity values that both surpass 80%. But a 3-item 3-region index of ”chronic inflammatory back pain” and two one-question items (Table 2) show 83.1% sensitivity and 86.4% specificity with likelihood ratios >5, if any 2 of 3 index items are met.
Conclusion: We propose a simple 3-item index assessing complaints at 3 regions that might be a useful tool to better define and classify the “Gestalt” of AS/axSpA, and also to improve the specificity of the current classification criteria. Validation of our results is needed in other data sets.
To cite this abstract in AMA style:
van der Linden S, Li Z, Brown M, Villiger P, Baumberger H, Zandwijk H, Khan M. Clinical History as Tool for Diagnosis and Classification of Patients with Ankylosing Spondylitis (Axial Spondyloarthritis): Evidence from a 35-Year Follow-up Family Study of a Swiss Cohort [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/clinical-history-as-tool-for-diagnosis-and-classification-of-patients-with-ankylosing-spondylitis-axial-spondyloarthritis-evidence-from-a-35-year-follow-up-family-study-of-a-swiss-cohort/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-history-as-tool-for-diagnosis-and-classification-of-patients-with-ankylosing-spondylitis-axial-spondyloarthritis-evidence-from-a-35-year-follow-up-family-study-of-a-swiss-cohort/