Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: The COVID-19 pandemic created an urgent need for access to care while preserving patient safety through social distancing. Prior to the pandemic, patients were seen solely face to face for all visits in our academic practice, consisting of 17 rheumatologists and 5 advanced practice providers. We utilized quality improvement (QI) methods in rapid cycles to accelerate telehealth implementation and report our outcomes and lessons learned in this process to guide future telehealth efforts.
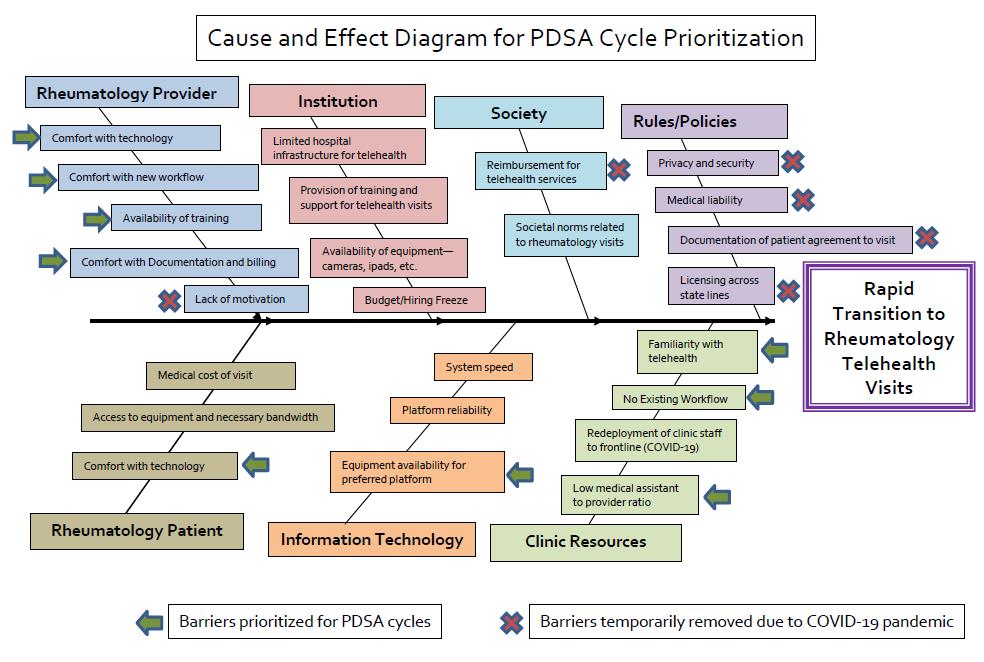
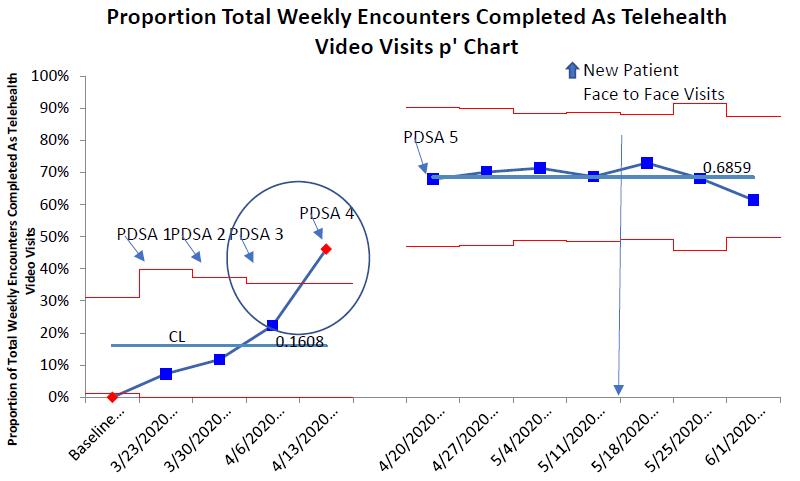
Methods: An inter-professional rheumatology telehealth team was established. We utilized the Define-Measure-Analyze-Improve-Control framework, Lean Six Sigma tools, and project charter to design this project. The primary impact measures were to increase the percentage of rheumatology providers utilizing ³50% video for patient visits from 0 to 90% and to increase the percentage of video visits from 0 to 70% between 3/23/20 and 4/20/20. We aimed to maintain the measures while social distancing policies remained in effect (6/1/2020). Balancing measures included provider patient satisfaction scores and visit volume. Baseline data were obtained between 1/7/20 and 3/13/20. We used a cause and effect diagram and voice of the customer (point-of care observations and provider survey) to prioritize Plan-Do-Study-Act (PDSA) cycles and statistical process control p-charts for primary impact measure analysis using QI macros for Microsoft Excel.
Results: Cause and effect analysis indicated provider, staff, and patient education and restructuring of clinic resources as high priority areas for PDSA cycles, while policy barriers were temporarily removed (Figure 1). Weekly PDSA cycles included telehealth education, live demonstration, pre-visit workflow development, simplification, and standardization, respectively. In the baseline period, no telehealth visits occurred, weekly visit average was 473, and patient satisfaction score was 95 of 99. We achieved 95% of providers conducting ≥ 50% of visits as video and 70% of total weekly visits conducted by video by week 5, with the greatest increase attributed to PDSA cycles 3 and 4 (Figures 2 and 3). Measures were maintained for three additional weeks before a slight decline after new patient face-to-face visits were added 5/15/20. Provider patient satisfaction scores remained stable and total rheumatology visit volume decreased by 60% in the first week followed by a steady increase to baseline with video visits as the primary visit type. Provider survey identified three major barriers to telehealth implementation: patient access/ability to use telehealth, interstate licensing, and clinic staff support.
Conclusion: The temporary removal of policy barriers and use of QI methods facilitated rapid and robust telehealth implementation in our academic practice in the face of a pandemic. This process identified the development, simplification, and standardization of pre-visit telehealth workflow as crucial factors for rapid and sustained success and allowed recovery of visit volume, while maintaining patient satisfaction and safety. Future efforts will focus on hybrid clinic workflows that can be rapidly scaled while addressing patient and provider barriers to telehealth.
To cite this abstract in AMA style:
Thomas J, Lebiedz-Odrobina D, Register K, Ferrara F, Barlow D, Riddle A, Miller K. Lessons Learned Through Rapid Quality Improvement for Telehealth Implementation in an Academic Rheumatology Practice During the COVID-19 Pandemic [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/lessons-learned-through-rapid-quality-improvement-for-telehealth-implementation-in-an-academic-rheumatology-practice-during-the-covid-19-pandemic/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lessons-learned-through-rapid-quality-improvement-for-telehealth-implementation-in-an-academic-rheumatology-practice-during-the-covid-19-pandemic/