Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Immune checkpoint inhibitors (ICIs) target checkpoint proteins PD-1/PD-L1 and CTLA-4 to activate and enhance the cytotoxic effects of T lymphocytes against tumor cells [1-2]. This systemic effect disrupts immune homeostasis and can result in immune-related adverse events (irAEs) affecting a wide variety of organs, including rheumatic presentations. Interestingly, irAEs are also reflective of anti-tumor efficacy [3].
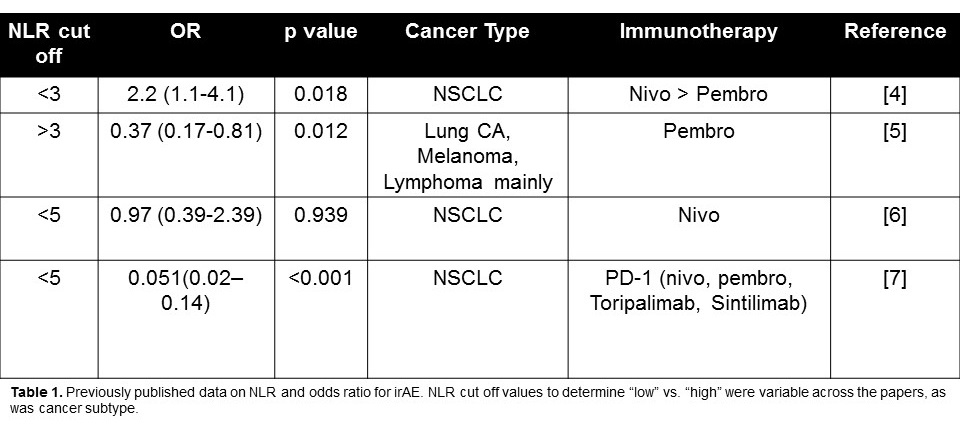
There are currently no biomarkers that predict impending irAEs. Several studies demonstrated an association between low neutrophil-to-lymphocyte ratio (NLR) and the risk of irAEs in patients treated with PD-1/PD-L1 blockade (Table 1). To date, the literature is limited on whether NLR may serve as a marker for irAEs in patients undergoing CTLA-4 blockade. As CTLA4 blockade affects a separate and distinct checkpoint pathway, we sought to understand the utility of NLR in this treatment group.
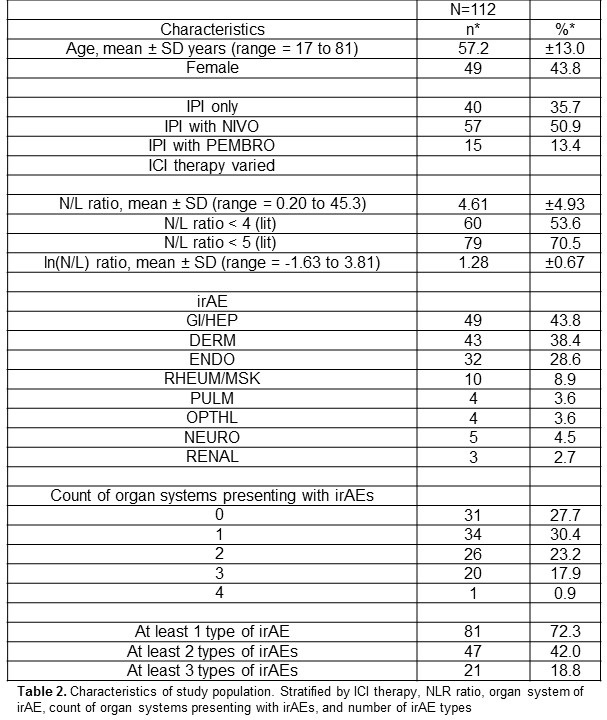
Methods: Under IRB approval, we conducted a retrospective electronic medical record review of oncology patients treated with ipilimumab (anti-CTLA4) at UNC Chapel Hill from 1/2004 to 7/2017. NLR was calculated from CBCs prior to initiation of ICI and compared against irAE type and incidence using logistic regression models to obtain odds ratios adjusted for age, sex, and ICI therapy type.
Results: 112 patients received ipilimumab (35.7% monotherapy with 64.3% in combination with other ICIs) and irAEs occurred in 72.3% of patients (Table 2). Lower NLR was shown to be associated with an increased risk of irAEs of any severity in patients treated with ipilimumab (Table 3). When stratifying irAEs by organ system, there was no statistically significant effect found. Despite this, the data suggest an association of NLR< 5 with rheumatologic irAEs. In addition, we noted an association of low NLR with dermatologic irAEs among women. While an exploratory endpoint, this difference between women and men is an intriguing finding not previously reported.
Conclusion: Our data investigating low NLR as a predictor for irAEs in CTLA-4 treated patients shows a similar association to that reported with PD-1 blockade. Furthermore, the effect size in our population is similar to previously published data with PD-1 blockade [4-7], suggesting this effect is not unique to cancer type or ICI type. The statistical significance was lost when stratified by organ system, suggesting a lack of power. Also of note is the difference in effect size based on NLR cut off value. To date, there is no standard value. While the data suggests NLR may be a predictor for irAE, it also encourages further investigation into organ specific irAEs, sex differences, and setting a standard for NLR cut off.
To cite this abstract in AMA style:
Cunningham M, Alvarez C, Saxena Beem S, Schwartz T, Ishizawar R. Neutrophil to Lymphocyte Ratio as a Predictor of Immune-Related Adverse Events in CTLA-4 Treated Patients: A Retrospective Review [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/neutrophil-to-lymphocyte-ratio-as-a-predictor-of-immune-related-adverse-events-in-ctla-4-treated-patients-a-retrospective-review/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/neutrophil-to-lymphocyte-ratio-as-a-predictor-of-immune-related-adverse-events-in-ctla-4-treated-patients-a-retrospective-review/