Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Incapacitating inflammatory arthritis occurs in up to 88% of patients with systemic lupus erythematosus (SLE). Arthritis is present in 70-80% of lupus patients in clinical trials. There is continued debate as to whether tenderness in the absence of swelling constitutes active lupus arthritis and should be scored on activity instruments. The confusion over arthritis scoring impacts clinical care and trials. There is an unmet need for a simple tool that can objectively assess lupus arthritis; near-infrared optical imaging has the potential to address this need. Over the last decade the technology has been optimized for use in brain imaging, breast cancer, and peripheral ischemia. Studies have also shown its utility in rheumatoid arthritis. Near-infrared light illuminates the tissues and transmitted and reflected light intensities are measured. Maps computed from these measurements show the spatial distribution of physiological parameters. Changes in optical properties caused by physiologic changes form the basis for its diagnostic capabilities. Using a so-called frequency-domain optical imaging (FDOI) system1 we evaluated the proximal interphalangeal (PIP) joints of 16 SLE patients and 10 healthy volunteers.
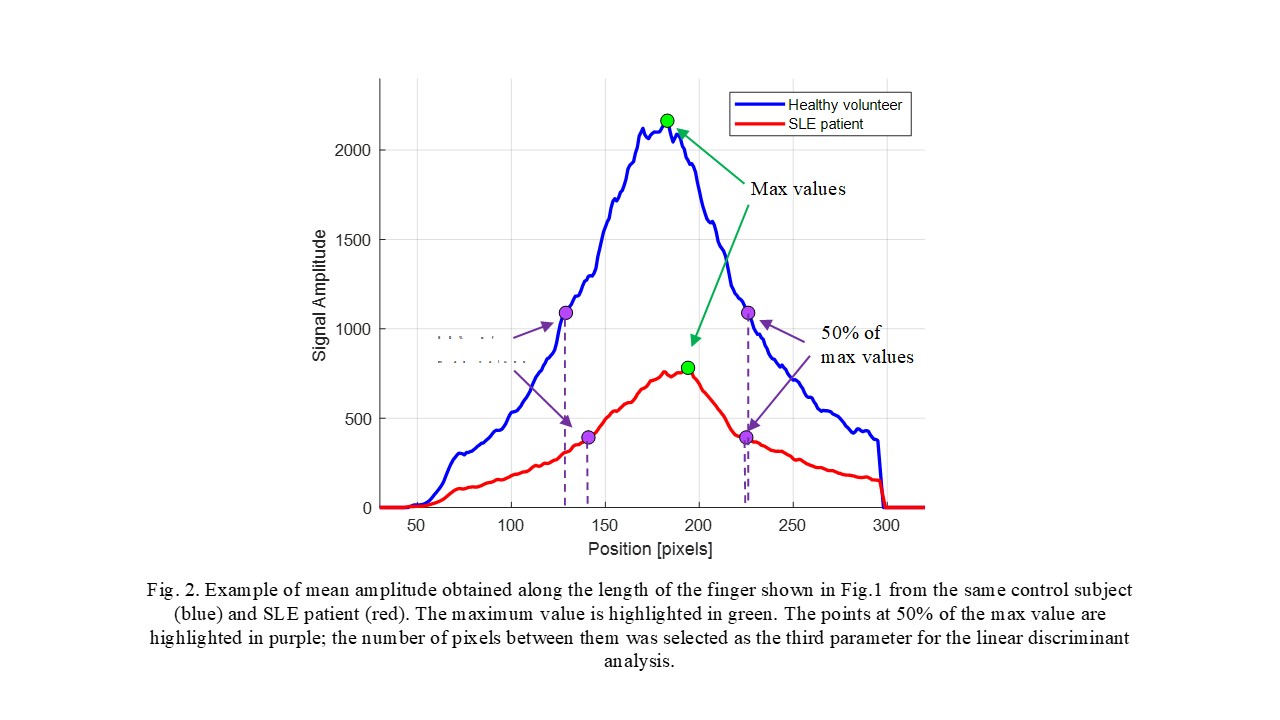
Methods: The FDOI system consists of a laser diode projecting a 1-mm – 670nm optical beam at 11 different positions along the PIP joints, 2mm apart, lengthwise. Fig.1 shows with the positions of the source. At each point, 16 images are acquired at different phases by a camera. The FDOI system is operated at a frequency of 300 MHz. PIPs 2-4 bilaterally were evaluated. A total of 60 healthy joints from 10 healthy volunteers and 96 joints from 16 patients with SLE arthritis were analyzed. Amplitudes and phases signals were generated using a demodulation algorithm.1 The fingers’ sizes (width and thickness) were measured using a caliper.
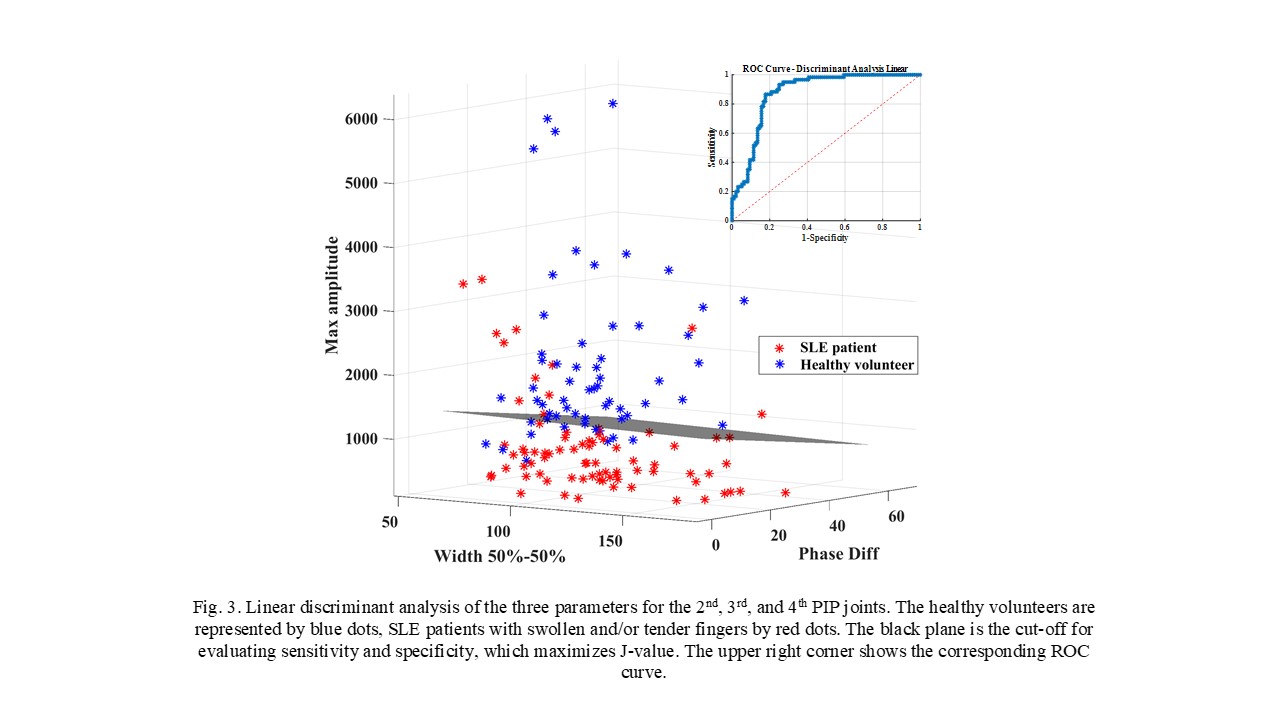
Results: The 16 patients with SLE arthritis (94% women, mean age 43±10 years, disease duration 14±8 years) had 74 swollen and/or tender PIP joints. Considering the mean signals from the 11 illumination positions (see Figs. 1 and 2), a discriminant analysis was done considering three variables: the maximum amplitude at the peak of the curve obtained, the maximum difference of the phase signals, and the number of pixels between 50% of the maximum value on the left and on the right of the peak. A receiver-operating curve (ROC) analysis showed an area under the curve (AUC) of 0.88 with correspondent sensitivity of 87% and specificity of 80% (Fig. 3).
Conclusion: These pilot data show that FDOI measurements of the PIP joints provide a clear difference between SLE patients and healthy subjects. If confirmed in a larger clinical study, FDOI could bring objectivity to the quantification of SLE arthritis. Compared to joint counts, US, and MR imaging, the advantages of FDOI are non-invasiveness, objectivity (eliminates inter-rater variability and operator dependency), low cost, and high speed of performance (~5 min).
To cite this abstract in AMA style:
Tang W, Marone A, Kim Y, Chen T, Guo C, Khalili L, Hielscher A, Askanase A. Optical Tomography Can Accurately Diagnose Lupus Arthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/optical-tomography-can-accurately-diagnose-lupus-arthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/optical-tomography-can-accurately-diagnose-lupus-arthritis/