Session Information
Session Type: Abstract Session
Session Time: 3:00PM-3:50PM
Background/Purpose: Previous analyses in the Nurses’ Health Study (NHS) cohorts have shown that eating a healthier diet, as measured by the Alternative Healthy Eating Index (AHEI), is associated with a reduced risk of rheumatoid arthritis (RA) particularly seropositive RA, among younger women. Here, we used a marginal structural model (MSM) approach to determine potential thresholds of dietary improvement on the risk of RA in women.
Methods: We followed 83,585 women in the NHS II (1995-2017) prospective study cohort, where information on lifestyle, diet, and health was obtained biennially through validated questionnaires. We fitted an MSM via weighted pooled logistic regression with inverse-probability-of-censoring and exposure weights to approximately calculate risk ratios (RR) and 95% confidence intervals (CI). The models were adjusted for baseline and time-varying covariates including age,body mass index, smoking, age at menarche, parity and breastfeeding status, menopausal status and hormone use, census tract median family income, prior diet, and total energy intake. Diet quality and risk of incident RA were investigated using dichotomous cut-points of AHEI score (cut-points: 60, 65, 70, 75; AHEI score ranged from 0, which represented the least healthy diet, to 110, which represented the healthiest diet) (Table 2).
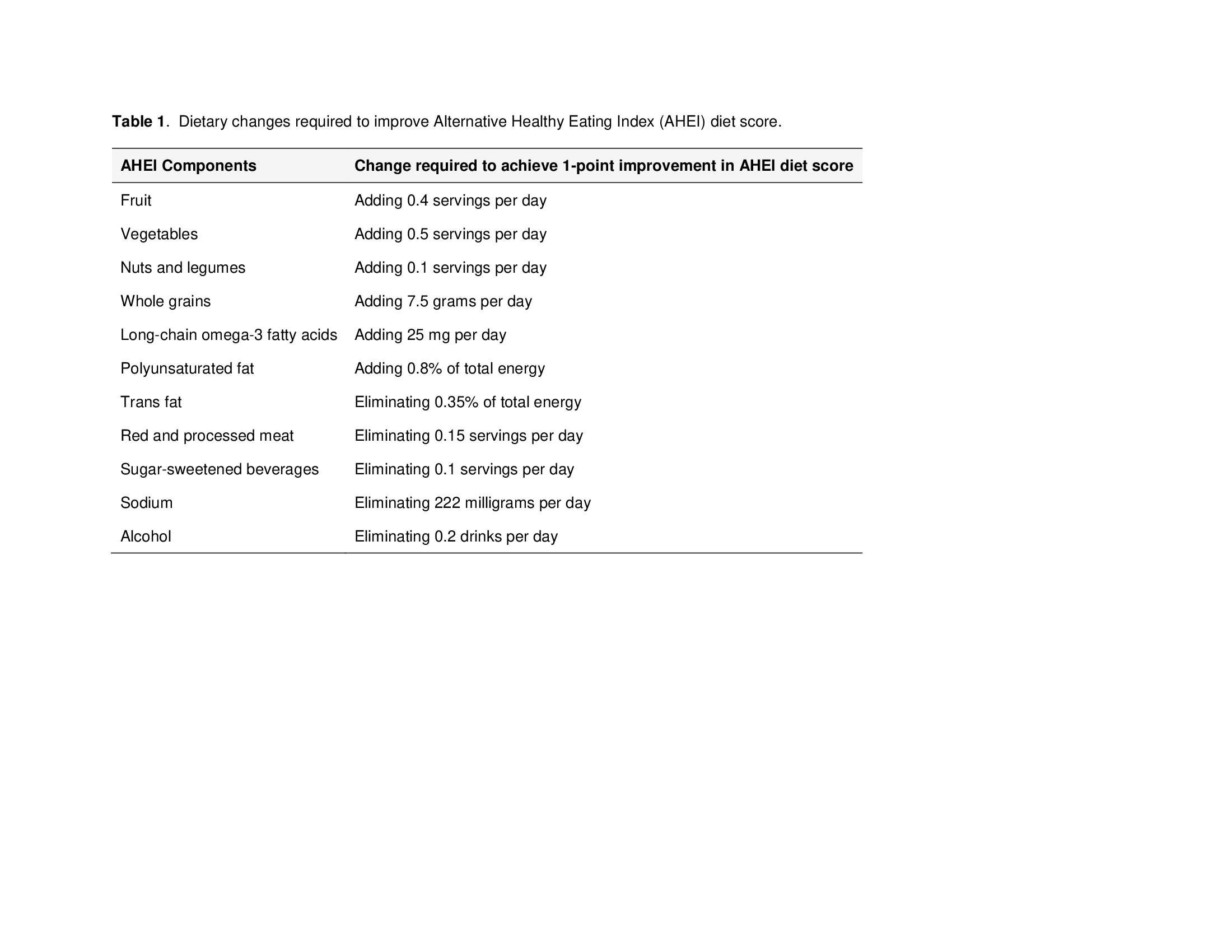
Results: Over 1,475,223 person years, there were 337 confirmed incident cases of RA. At baseline, the mean age was 40.3 years (SD ±4.6) and the mean AHEI score was 57.1 points (SD ±13.8). During 22 years of follow-up there was a mean AHEI score improvement of 9.1 points (SD ±12.7). The risk of RA, comparing long-term adherence to an AHEI score of at least 75 points with maintaining dietary quality below this threshold, was reduced by more than 50% (RR 0.43; 95% CI 0.27, 0.67) (Table 1). Risk reduction was similar for seropositive RA (RR 0.41; 95% CI 0.22, 0.74) and seronegative RA (RR 0.47; 95% CI 0.25, 0.91) (Table 1). Maintaining AHEI scores below the threshold of 75 was not associated with a reduced risk of RA.
Conclusion: Our results suggest that adherence to higher diet quality at an AHEI threshold score of ≥75 points may lower the risk of RA by more than 50% in women. Such an improvement could be achieved by increasing fruit, vegetable, nut, legume, whole grain, omega-3, or polyunsaturated fat consumption, or by decreasing sodium, sugar-sweetened beverage, or red/processed meat consumption.
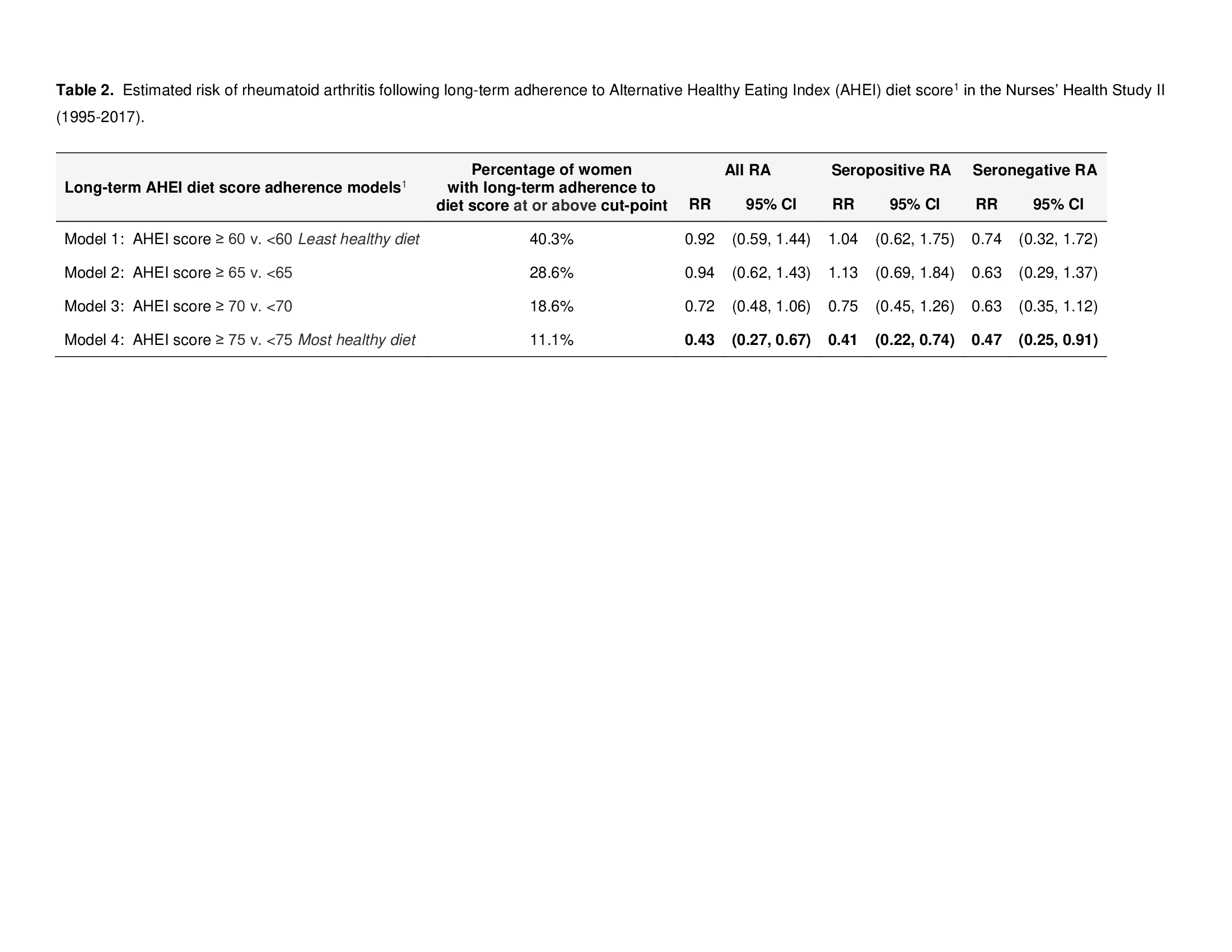 1. Higher score indicates healthier diet (AHEI diet score range: 0-110) 2. Adjusted for baseline pervious AHEI score (continuous), age at menarche (12 months breastfeeding), menopausal status and hormone use (pre-menopausal, post-menopausal with never use, current use and past use), census tract median family income (quartiles), and total energy (quintiles).
1. Higher score indicates healthier diet (AHEI diet score range: 0-110) 2. Adjusted for baseline pervious AHEI score (continuous), age at menarche (12 months breastfeeding), menopausal status and hormone use (pre-menopausal, post-menopausal with never use, current use and past use), census tract median family income (quartiles), and total energy (quintiles).
To cite this abstract in AMA style:
Marchand N, Chiu Y, Yoshida K, Malspeis S, Sparks J, Costenbader K, Karlson E, Lu B. Threshold Level for Long-term Healthy Diet Adherence to Reduce the Risk of Rheumatoid Arthritis Among Women in a Prospective Cohort Using a Marginal Structural Model Approach [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/threshold-level-for-long-term-healthy-diet-adherence-to-reduce-the-risk-of-rheumatoid-arthritis-among-women-in-a-prospective-cohort-using-a-marginal-structural-model-approach/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/threshold-level-for-long-term-healthy-diet-adherence-to-reduce-the-risk-of-rheumatoid-arthritis-among-women-in-a-prospective-cohort-using-a-marginal-structural-model-approach/