Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Almost 40% of patients with SLE have comorbid mental health conditions.1 Though depression is most commonly reported (24% to 30%), many SLE patients also experience some form of anxiety disorder.2 The mechanisms underlying the association of psychiatric disorders with neuropsychiatric SLE are unclear. Moreover, the relationship between the longitudinal course of anxiety symptomology and SLE disease activity remains largely unstudied. Thus, the aims of this study are to identify patterns of anxiety symptomology over time among patients with SLE, and to assess the longitudinal relationship between anxiety symptomology and SLE disease activity.
Methods: Longitudinal data from patients with ACR or SLICC-classified SLE treated in the Washington University Lupus Clinic were analyzed. Anxiety symptomology was assessed at each visit using the validated Patient-Reported Outcomes Measurement Information System (PROMIS) Emotional Distress: Anxiety Short Form 8a. Patients with at least 3 PROMIS anxiety and SLEDAI2K Responder Index-50 scores obtained at the same clinic visit over 2 to 48 months were included. The PROMIS anxiety scale scores are converted to t-scores with a mean of 50, reflecting average levels of anxiety in the general adult population, with standard deviation of 10.3 T-scores between 60-70 and above 70 reflect moderate and severe symptomology, respectively. Group-based trajectory modeling (GBTM) identified groups of patients with similar temporal trajectories of anxiety symptomology. Baseline characteristics of individuals in each anxiety trajectory group were compared using chi-square tests, Fisher’s exact tests, or ANOVA. The relationship between disease activity and anxiety over time was assessed using multilevel linear regression models.
Results: 139 patients had at least 3 PROMIS anxiety scores over an average of 30.9 months (SD: 13.0; range: 2.6-48). Mean patient age was 40.2 (SD: 12.7; range: 19-74), 90.1% were female and 56.1% African American. GBTM identified 4 unique temporal trajectories of anxiety symptomology (Figure 1), labeled: low (LA), average (AA), moderate (MA), and high anxiety (HA). Of note, 88.9% of individuals classified in the HA group were African-American, compared to only 44.4% of individuals in the LA group (Table 1). SLEDAI score was not significantly associated with anxiety levels longitudinally (β=0.07, p=0.3).
Conclusion: Anxiety symptomology over time remained relatively stable in this patient cohort. More than 50% of patients experienced persistent moderate or severe anxiety symptomology, and a higher proportion of African-American patients demonstrated moderate or severe anxiety. SLE disease activity was not significantly associated with anxiety symptomology over time. These findings emphasize the importance of better understanding psychosocial factors that contribute to the persistence of anxiety symptomology. Patients with SLE should be regularly screened for mental health conditions and provided access to appropriate mental health resources.
1 Seawell, A. H., et al. Lupus, 2004. 13(12): 891–899.
2 Zhang, L., et al. BMC Psychiatry, 2017. 17(1): 70.
3 Pilkonis PA, et al. Assessment. 2011;18(3):263‐283.
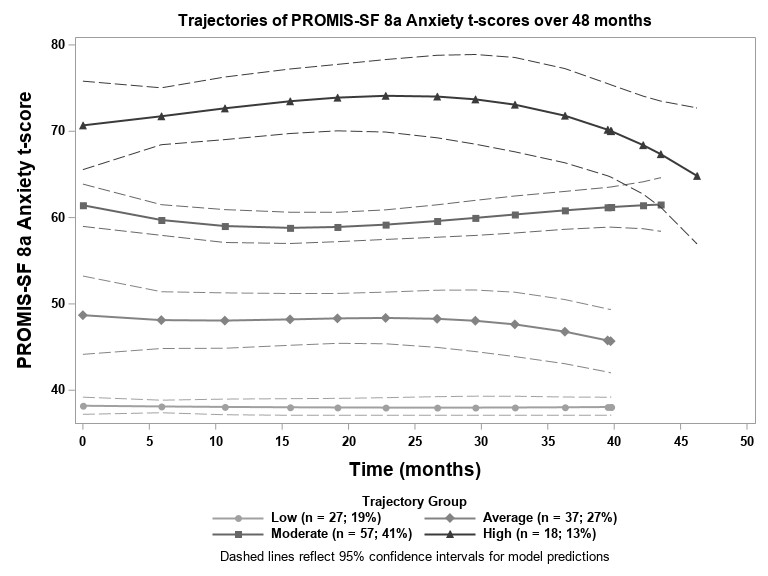 Figure 1. Identified trajectories of anxiety scores over time
Figure 1. Identified trajectories of anxiety scores over time
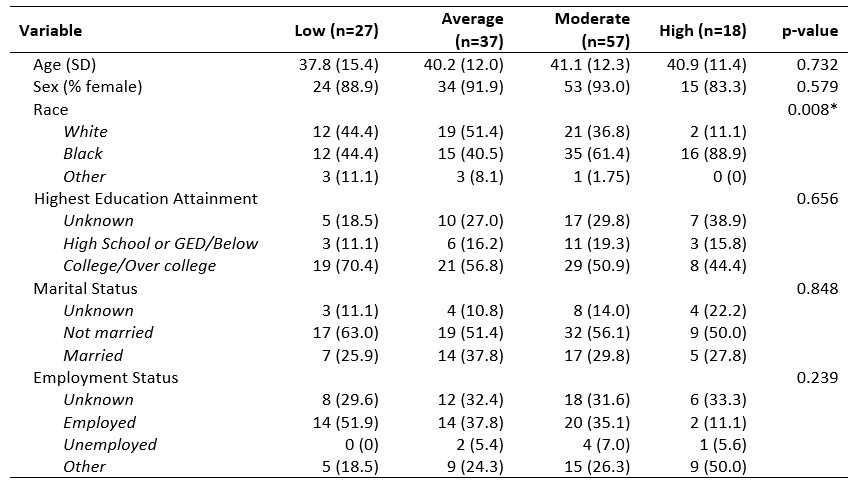 Table 1. Baseline sociodemographic characteristics of patients in each of the identified anxiety trajectory groups * Statistically significant at p < 0.05
Table 1. Baseline sociodemographic characteristics of patients in each of the identified anxiety trajectory groups * Statistically significant at p < 0.05
To cite this abstract in AMA style:
Lew D, Huang X, Kellahan S, Xian H, Eisen S, Kim A. Longitudinal Patterns of Anxiety Symptomology Among Patients with Systemic Lupus Erythematosus (SLE) Remain Stable over Time and Do Not Associate with SLE Disease Activity [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/longitudinal-patterns-of-anxiety-symptomology-among-patients-with-systemic-lupus-erythematosus-sle-remain-stable-over-time-and-do-not-associate-with-sle-disease-activity/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/longitudinal-patterns-of-anxiety-symptomology-among-patients-with-systemic-lupus-erythematosus-sle-remain-stable-over-time-and-do-not-associate-with-sle-disease-activity/
