Session Information
Date: Sunday, November 8, 2020
Title: RA – Diagnosis, Manifestations, & Outcomes Poster III: Cardiopulmonary Aspects
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Extra-articular manifestations of rheumatoid arthritis (RA), such as nodules and interstitial lung disease (ILD), portend poor outcomes and are more common in men than in women. Whether differences in the risk of RA-ILD between men and women are related to biologic sex or to other known risk factors such as cigarette smoking or increased RA disease activity, which might differ by sex, is unknown. The purpose of this cross-sectional study was to evaluate sex differences in the prevalence of extra-articular manifestations in RA, accounting for known factors that might confound these associations.
Methods: Participants were enrollees in a multicenter, longitudinal observational cohort of US Veterans with RA. A total of 2,691 participants were studied. Baseline demographic, clinical, and treatment variables were collected and compared between men and women using either Student’s t-tests or chi-square tests. Participants were categorized by the presence or absence of subcutaneous nodules, chronic lung disease (ILD or chronic obstructive pulmonary disease [COPD] vs. ILD alone) and ILD. Chronic lung diseases were determined from diagnostic codes recorded by treating rheumatologists at enrollment. Associations of sex (male vs. female) with each extra-articular manifestation was assessed using separate multivariable logistic regression models. Covariates included; Model 1: age; Model 2: age, race, body mass index (BMI); Model 3: age, race, BMI, measures of disease activity and RA treatments; Model 4: all aforementioned covariates and HLA-DRB1 shared epitope status, smoking history, and anti-citrullinated protein antibody (ACPA) status.
Results: Baseline characteristics of men and women with RA are shown in (Table 1). Compared to women with RA, men were older, more likely to be Caucasian, smokers, and had greater disease activity, higher autoantibody concentrations and more comorbidity. Men more often had nodules (28% vs. 19%, p = 0.001), COPD (17% vs. 10%, p = 0.004) and ILD (4.7% vs. 1.0%, p = 0.002). In hierarchical regression models, these sex differences all remained following adjustment for age (Table 2, Model 1). With progressive adjustments (Table 2, Models 2 to 4), associations between sex and nodules or chronic lung disease were attenuated and no longer significant. In contrast, associations of male sex with ILD alone remained following progressive adjustments. Results were unchanged in more parsimonious models including only age, smoking, disease activity and ACPA positivity as covariates (data not shown).
Conclusion: The association between subcutaneous nodules and chronic lung disease with male sex in RA is confounded by other factors, rather than representing true differences arising from biologic sex. In contrast, associations of biologic sex with RA-ILD persist even after adjustment for multiple confounders, including cigarette smoking, RA disease activity and/or severity, and treatments. Our findings suggest that real sex differences drive the marked differences observed in RA-ILD prevalence in men compared to women. Further exploration into mechanisms underpinning the predisposition to RA-ILD among men is needed as this could inform future preventive and/or treatment strategies.
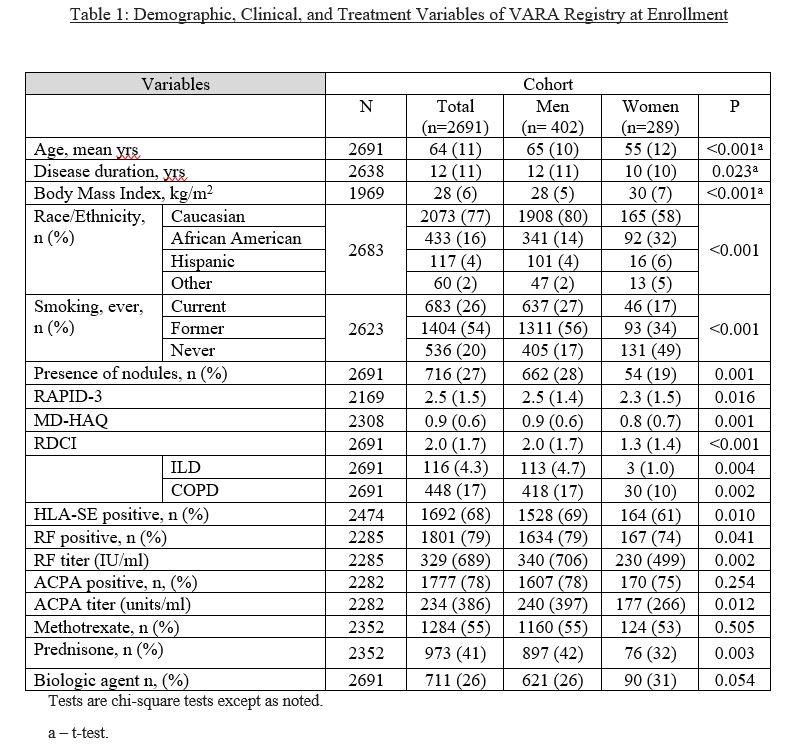 * RAPID-3: Routine Assessment of Patient Index Data; MD-HAQ: Multidimensional Health Assessment Questionnaire; RDCI: rheumatic disease comorbidity index; ILD: interstitial lung disease; COPD: chronic obstructive pulmonary disease; HLA-SE: human leukocyte antigen shared epitope; RF: rheumatoid factor; ACPA: anti-citrullinated peptide antibodies
* RAPID-3: Routine Assessment of Patient Index Data; MD-HAQ: Multidimensional Health Assessment Questionnaire; RDCI: rheumatic disease comorbidity index; ILD: interstitial lung disease; COPD: chronic obstructive pulmonary disease; HLA-SE: human leukocyte antigen shared epitope; RF: rheumatoid factor; ACPA: anti-citrullinated peptide antibodies
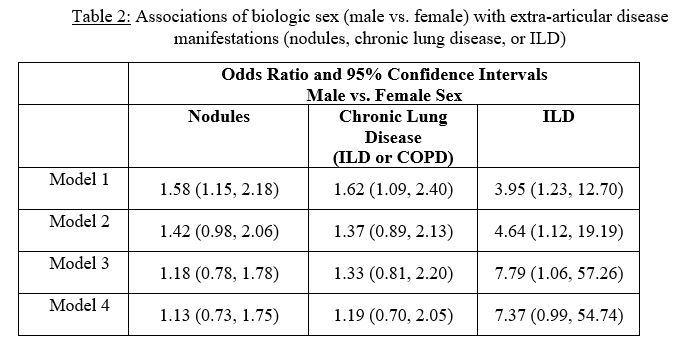 Covariates: Model 1 = age Model 2 = age, race, BMI Model 3 = age, race, BMI, disease duration, RAPID-3, MTX, prednisone, biologic therapy Model 4 = age, sex, race, BMI, disease duration, RAPID-3, MTX, prednisone, biologic therapy, HLA-DRB1 (pos vs. neg), smoking (ever vs. never), ACPA positivity
Covariates: Model 1 = age Model 2 = age, race, BMI Model 3 = age, race, BMI, disease duration, RAPID-3, MTX, prednisone, biologic therapy Model 4 = age, sex, race, BMI, disease duration, RAPID-3, MTX, prednisone, biologic therapy, HLA-DRB1 (pos vs. neg), smoking (ever vs. never), ACPA positivity
To cite this abstract in AMA style:
Wheeler A, Kerr G, Jileaeva I, Krishna A, England B, Sayles H, Thiele G, Poole J, Petro A, Mikuls T. Associations of Biological Sex with Interstitial Lung Disease in Patients with Rheumatoid Arthritis Are Independent of Other Known Risk Factors [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/associations-of-biological-sex-with-interstitial-lung-disease-in-patients-with-rheumatoid-arthritis-are-independent-of-other-known-risk-factors/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-of-biological-sex-with-interstitial-lung-disease-in-patients-with-rheumatoid-arthritis-are-independent-of-other-known-risk-factors/
