Session Information
Date: Sunday, November 8, 2020
Title: Patient Outcomes, Preferences, & Attitudes Poster II: Miscellaneous Rheumatic Diseases
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Frailty is associated with poor health outcomes in the general population, and recent studies have highlighted its importance in rheumatic musculoskeletal diseases (RMDs). Prior studies have found associations between frailty and low bone mineral density and fractures in RA and mortality in SLE and OA. These studies used performance or comorbidity-based measures of frailty which may not be feasible to collect in routine clinical care. Self-reported measures of frailty are validated in the general population but have not been widely studied in RMDs. We aimed to describe the prevalence of self-reported frailty across RMDs and to determine factors associated with frailty in a large observational cohort.
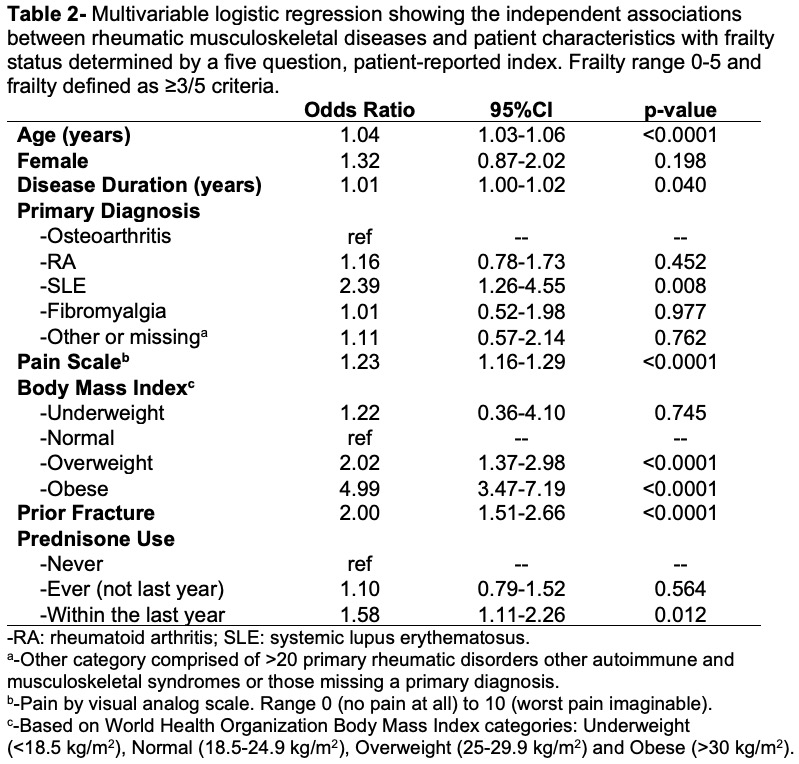
Methods: Data were from participants in FORWARD, The National Databank for Rheumatic Diseases, an observational longitudinal US-cohort registry with biannual patient questionnaires since 1998. The most recent wave of questionnaires, released in January 2020, included a 5-item validated patient-reported frailty index1. Participants were asked to report levels of fatigue, ability to walk several blocks, ability to climb ten stairs, weight loss, and presence of 11 comorbidities. Those meeting ≥3 of 5 criteria were categorized as frail. This analysis included all responses collected as of June 5, 2020. Multivariable logistic regression analysis was performed to identify factors independently associated with frailty.
Results: 1423 responses were included in this analysis, 63% with RA, 15% with OA, 7% with SLE, 4% with FM and 11% with other/unknown RMDs. Those categorized as frail (N=420, 30%) were older, had longer disease duration, greater pain, and were more likely to be obese (Table 1). The frail group reported a higher frequency of prednisone use in the last year as compared to the non-frail group (26% vs. 16%) but reported similar ever and never use of prednisone. The frail group reported more historical fractures than those who were not frail. SLE had the highest proportion of frailty (39%) despite being the youngest group (61±12 years). The top three factors contributing to frailty scores were inability to walk several blocks, inability to climb 10 stairs, and ³5/11 comorbidities (Table 1). In the multivariable model, age, disease duration, pain scale, prednisone use within the last year, and prior fracture were associated with elevated odds ratios of frailty (ORs 1.04, 1.01, 1.23, 1.58 and 2.02 respectively, all p< 0.05) (Table 2). Within RMDs, using OA as the reference group, SLE was associated with 2.39-fold greater odds of frailty (p=0.008). Using normal weight as the referent, overweight and obesity were also associated with a greater odds of frailty (ORs 2.02 and 4.99, p< 0.0001).
Conclusion: Self-reported frailty was prevalent in a third of participants with RMDs, with the highest rate in those with SLE despite that group having the lowest age. SLE, prior fracture, prednisone use within the last year, and obesity had the greatest odds of frailty in the multivariable model. Future longitudinal analyses to determine factors associated with incident frailty and its sequelae are needed in this high-risk population.
1. Morley et al, J Nutr Health Aging. 2012;16(7):601
To cite this abstract in AMA style:
Wysham K, Baker J, Wipfler K, Lieber S, Sattui S, Katz P, Michaud K. Prevalence of Frailty and Associated Factors in a National Observational Cohort of Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/prevalence-of-frailty-and-associated-factors-in-a-national-observational-cohort-of-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-frailty-and-associated-factors-in-a-national-observational-cohort-of-rheumatic-diseases/