Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Osteoarthritis (OA) is a mechanically and immunologically mediated common disease with a complex pathogenesis. Despite epidemiologic studies proving increasing age, obesity and female gender as risk factors, many individuals are unable to manage OA symptoms and optimal treatment strategies at a population health level remain a challenge. Our aim was to determine prevalence, incidence and characteristics of OA patients over an 18-year timeframe to provide insight into what treatments and preventative strategies would maximize impact.
Methods: This was a retrospective descriptive study reviewing electronic health records and billing data at Geisinger, an integrated health system in central and northeastern Pennsylvania serving over 500,000 patients per year. Patients were included if they had at least two outpatient encounters at age 18 or greater and defined as having OA after having at least one diagnosis code for OA (ICD-9: 715.*, ICD-10 M15-19) on a problem list or encounter diagnosis or had an OA-related procedure (hip or knee replacement, arthroscopy or injection). Patients with total knee replacement (TKR) were also examined separately as a subset. For each year from 2001-2018, we calculated OA prevalence (percent of patients seen with OA) and incidence (percent of patients newly diagnosed with OA that year). We also examined baseline demographics, OA-related prescription medication use, and comorbidities at any time during the study period.
Results: We identified 271,126 patients with encounters in the health system and evidence of OA, representing 32% of the total patient population in 2018. Yearly incidence remained steady over the past 10 years at between 4 and 5 newly diagnosed per 100 and was similar between males and females. The cohort remained steady at approximately 60% female, and consistent with the geographic region, was 98% Caucasian and non-Hispanic. The largest segment of the OA population was in the range of 45 to 64 years old at first encounter, but the youngest age segment (18-45 years old) increased from 20% to 25% of the OA population over the study period. Over half (54%) of OA patients had a BMI over 30 and this percentage increased by 7% since 2001. Non-tramadol opioids were the most commonly prescribed pain medications, followed by acetaminophen (prescription or over-the-counter) and oral non-steroidal anti-inflammatory drugs. Depression and anxiety disorders were diagnosed in 17% and 20% of the OA population, respectively, 20% reported chronic obstructive pulmonary disease, and 46% reported current or past tobacco smoking. Approximately 4% of patients underwent TKR; this subgroup was more likely to use prescription pain medication and had higher rates of several chronic diseases including congestive heart failure, hypertension and chronic kidney disease.
Conclusion: Osteoarthritis affected a large, increasing segment of a large health system population, with higher rates among females and the proportion of younger individuals increasing over time. The treatment of these patients may have been further complicated by comorbidities including obesity, depression, anxiety and multiple chronic disease states.
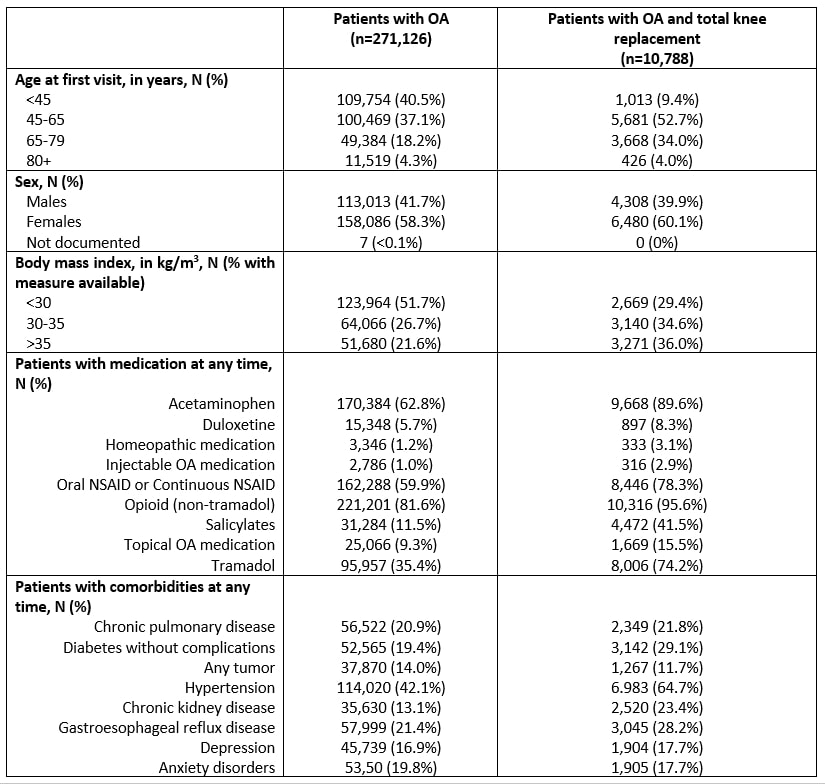 Demographics, Medications, and Comorbidities Table
Demographics, Medications, and Comorbidities Table
To cite this abstract in AMA style:
Graham J, Novosat T, Sun H, Piper B, Boscarino J, Kern M, Duboski V, Wright E, Schepman P, Robinson R, Casey E, Beck C, Hall J. Osteoarthritis in a Large Integrated Health System Population: 18-Year Retrospective Review [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/osteoarthritis-in-a-large-integrated-health-system-population-18-year-retrospective-review/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/osteoarthritis-in-a-large-integrated-health-system-population-18-year-retrospective-review/
