Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Interstitial lung disease (ILD) occurs in up to 80% of patients with dermatomyositis (DM) and polymyositis (PM), and is a leading cause of morbidity and mortality (Lung. 2016;194(5):733‐737). The current study validates the use of a computer aided diagnostic system to quantitatively score ILD on high-resolution computed tomography (HRCT) scans (Clin Exp Rheumatol 2010;28, S26-35) in a cohort of DM/PM patients. The predictive value of the baseline quantitative ILD score on change in lung function at follow-up is also examined.
Methods: HRCT images were retrospectively analyzed from DM/PM patients in our longitudinal myositis cohort who had thin-section, full inspiration images available for review. The QILD is the sum of all abnormally classified scores, which include quantitative scores for reticulations/fibrosis (QLF) and ground glass opacity (QGG). Quantitative ILD scores (QGG, QLF, QILD) were assessed for whole lung, and for zone of maximum involvement. Linear regression models were constructed in patients with DM/PM associated ILD, as well as in total DM/PM patients with QILD scores to evaluate the association between baseline variables including QILD scores and the relative change in forced vital capacity (FVC) at the follow-up visit. Change in FVC was calculated as the difference between most recent and baseline FVC divided by baseline FVC. Mean (SD) follow-up time between PFTs was 37(31) months.
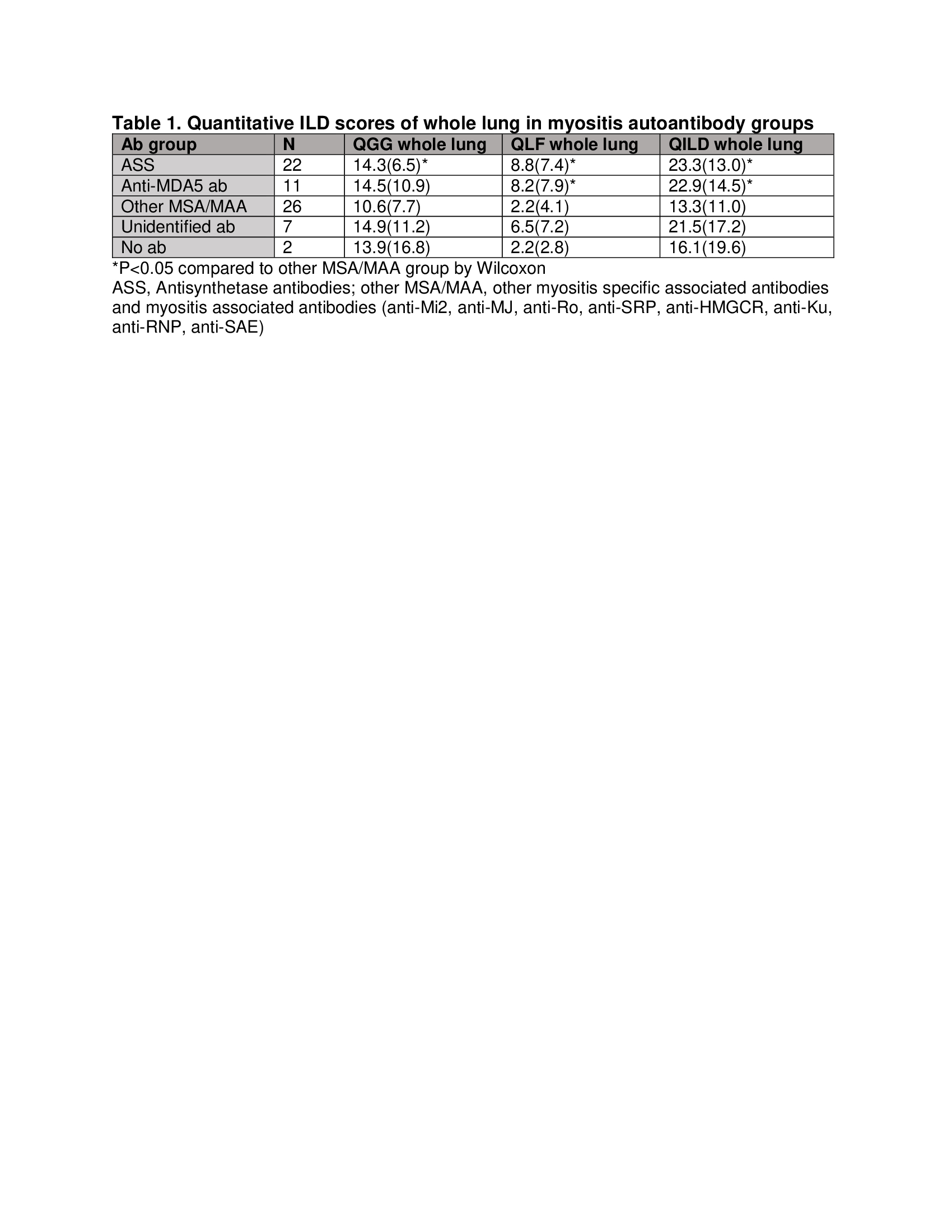
Results: A total of 72 DM/PM patients with baseline and follow-up HRCT scans were included in the analysis. Quantitative ILD scores showed predominance of ground glass rather than fibrosis with most of the involvement in lower lung zones, consistent with nonspecific interstitial pneumonia (NSIP) pattern. The quantitative ILD scores (QGG, QLF, QILD) demonstrated good concordance with lung physiology (FVC, TLC and DLCO) (correlation coefficient between -0.41 to -0.70, p< 0.001 for all). When analyzed by myositis autoantibody subgroups, patients with antisynthetase and anti-MDA5 antibodies had the highest fibrosis score (QLF) and total ILD score (QILD) (Table 1).
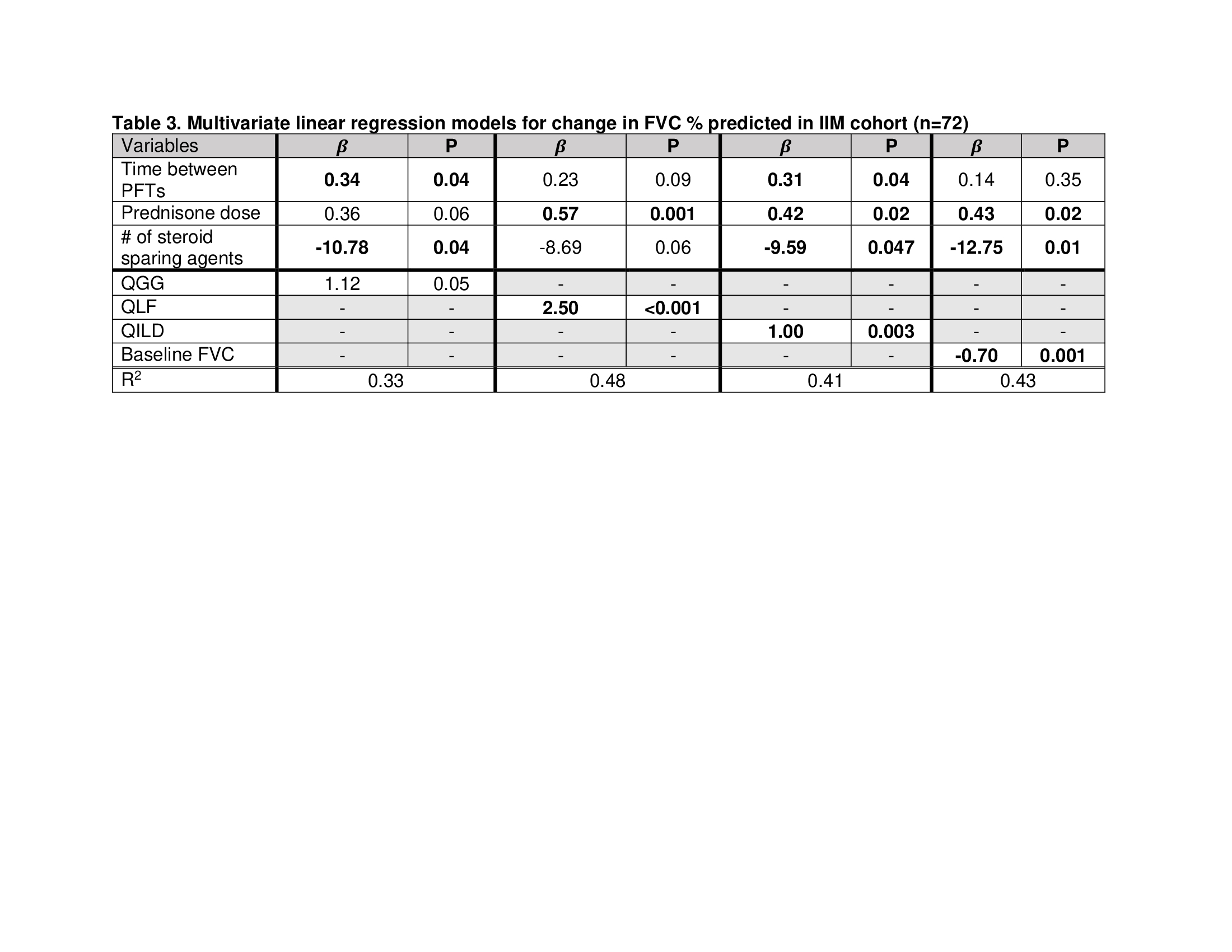
Linear regression models demonstrated that higher baseline quantitative ILD scores were associated with greater improvement in FVC at follow-up (Table 2). These relationships remained strong after multivariate adjustment of other baseline variables including baseline daily prednisone dose and number of steroid sparing agents (Table 3). The predictive value of QLF, QILD models assessed by R2 was comparable to the model using baseline FVC, suggesting quantitative ILD scores may be used as a quantitative outcome measure for DM/PM-ILD severity.
Conclusion: Quantitative ILD scores can provide an objective quantitative tool for assessing ILD severity in DM/PM-ILD and are associated with clinically meaningful longitudinal outcomes.
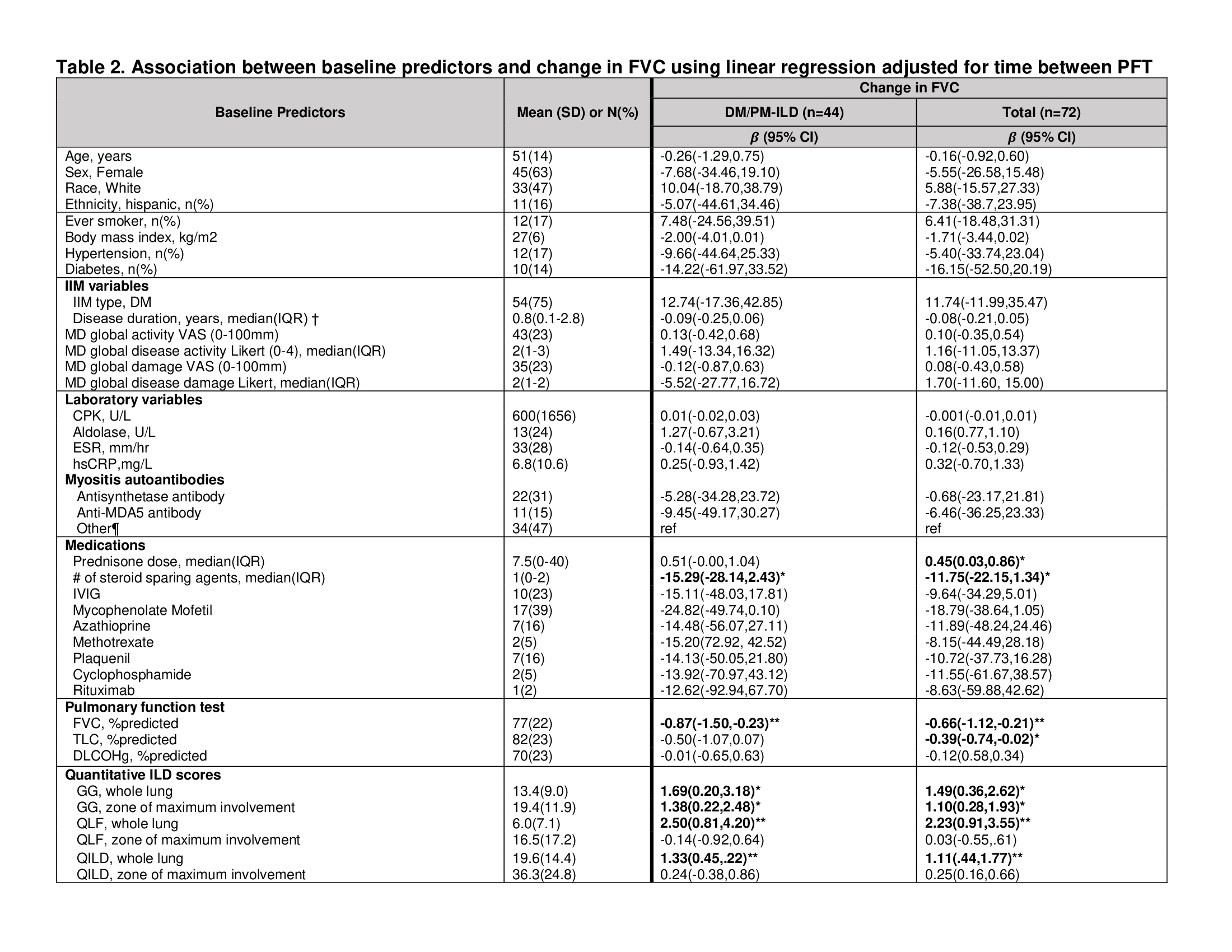 *p < 0.05 **p < 0.01 †DM/PM or ILD duration, whichever that started first ¶ MSA testing in 68/72 patients, other includes other MSA/MAA (Mi2 n=6, MJ n=5, Ro n=4, SRP n=4, HMGCR n=3, Ku n=1, RNP n=1, SAE n=1), unidentified ab (n=7) and no autoab (n=2)
*p < 0.05 **p < 0.01 †DM/PM or ILD duration, whichever that started first ¶ MSA testing in 68/72 patients, other includes other MSA/MAA (Mi2 n=6, MJ n=5, Ro n=4, SRP n=4, HMGCR n=3, Ku n=1, RNP n=1, SAE n=1), unidentified ab (n=7) and no autoab (n=2)
To cite this abstract in AMA style:
Bae S, Oh A, Kim G, Goldin J, Charles-Schoeman C. A Computer-Aided Diagnostic System for Quantitative Scoring of Extent of Interstitial Lung Disease (ILD) in Dermatomyositis/Polymyositis Associated ILD [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/a-computer-aided-diagnostic-system-for-quantitative-scoring-of-extent-of-interstitial-lung-disease-ild-in-dermatomyositis-polymyositis-associated-ild/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-computer-aided-diagnostic-system-for-quantitative-scoring-of-extent-of-interstitial-lung-disease-ild-in-dermatomyositis-polymyositis-associated-ild/