Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Patient-reported outcomes (PROs) are increasingly used in rheumatology. Such outcomes are under-reported in autoimmune inflammatory myopathies (AIM) especially in incident cohorts. The objective of this study was to explore physical function, fatigue, depressive symptoms, sleep quality and health-related quality of life (HRQoL) in early AIM, and the effect of disease activity on those domains.
Methods: Cross-sectional study of adult AIM subjects with disease duration of <2 years enrolled in a multicenter research cohort. Standardized clinical histories, medical examinations, and self-administered questionnaires were collected at baseline visit. Physical functioning was assessed using the Health Assessment Questionnaire (HAQ; scores from 0 (no disability) to 3 (severe disability)). Fatigue was measured using the Functional Assessment of Chronic Illness Therapy (FACIT; scores from 0-52, lower scores representing more fatigue). Depressive symptoms were assessed using the Patient Health Questionnaire (PHQ-9; scores from 0-27, higher scores representing worse symptoms). The PROMIS Short Form v1.0 – Fatigue 8a and the Medical Outcomes Trust Short Form-36 (SF-36) were used to assess sleep quality and HRQoL, respectively. Both are norm based, with mean scores of 50 and standard deviations (SD) of 10 (PROMIS, higher scores representing worse sleep quality; SF-36, lower scores representing worse HRQoL). Disease activity was measured by the recruiting physician using a numerical rating scale ranging from 0 (no activity) to 10 (maximum severity). Multivariate linear regression models were generated to determine the association between disease activity and PROs.
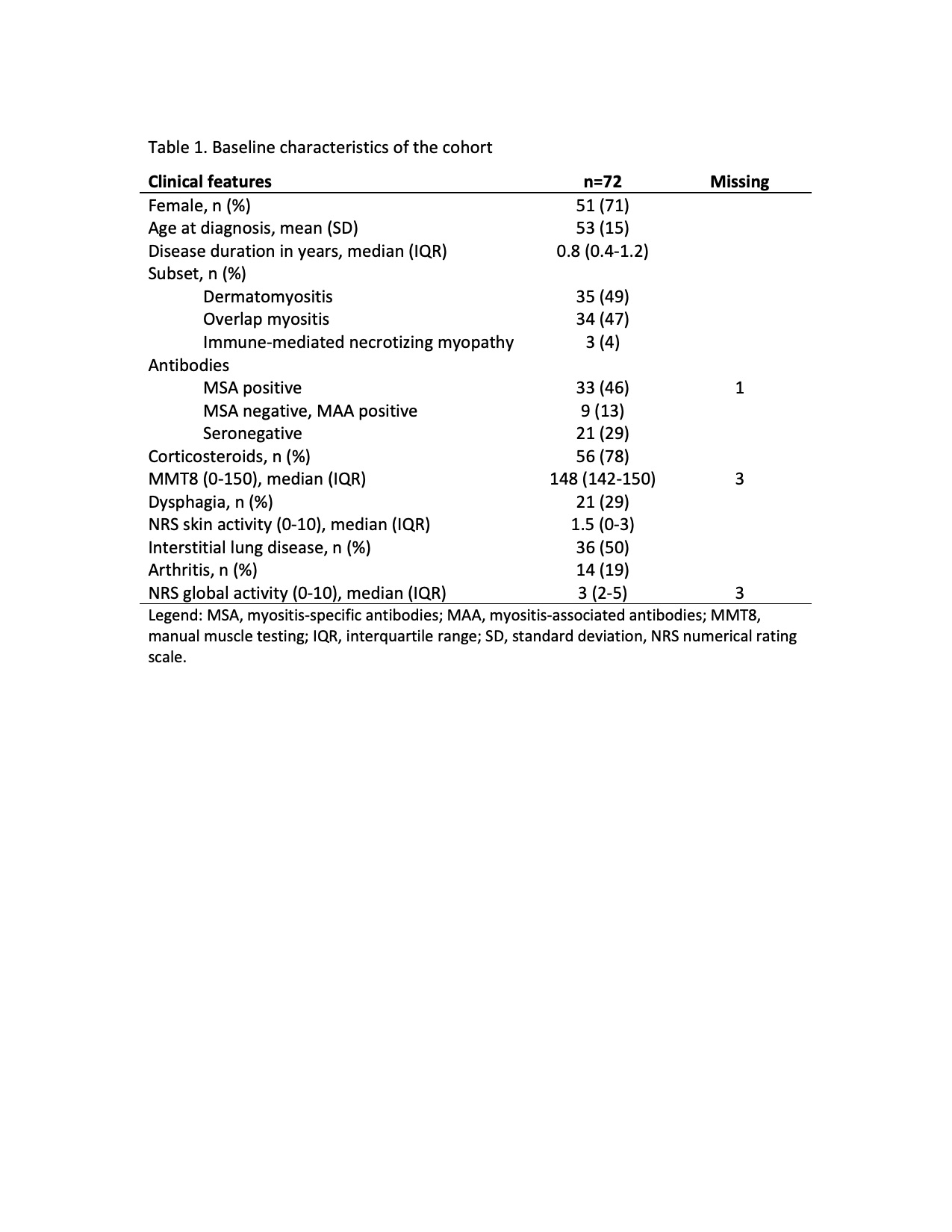
Results: The study included 72 AIM subjects (71% female, mean age 53 years, mean disease duration 0.8 years) with dermatomyositis (49%), overlap myositis (47%) and immune-mediated necrotizing myopathies (4%) (Table 1). Half of the subjects had interstitial lung disease, 29% dysphagia and 19% arthritis. Baseline median (IQR) disease activity was 3 (2-5).
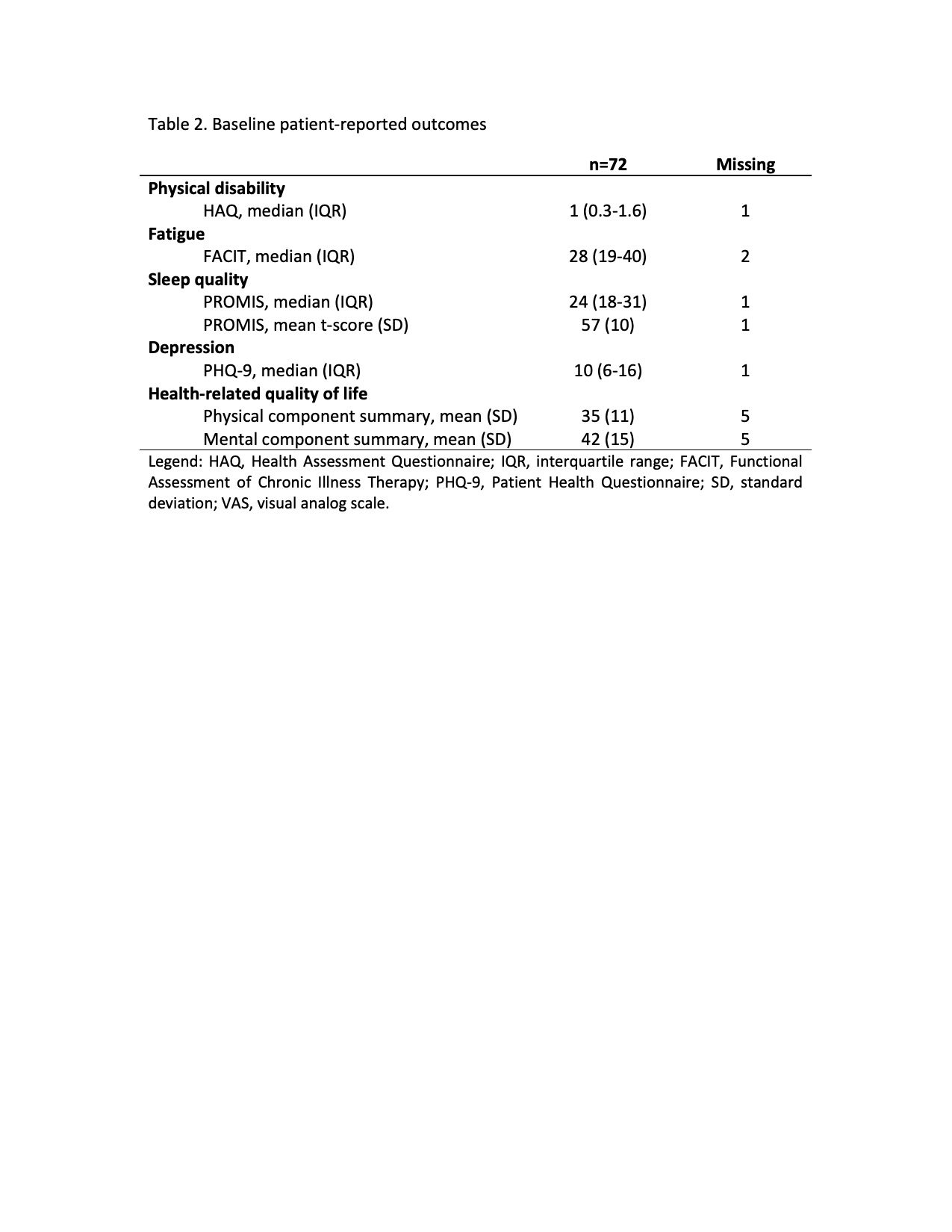
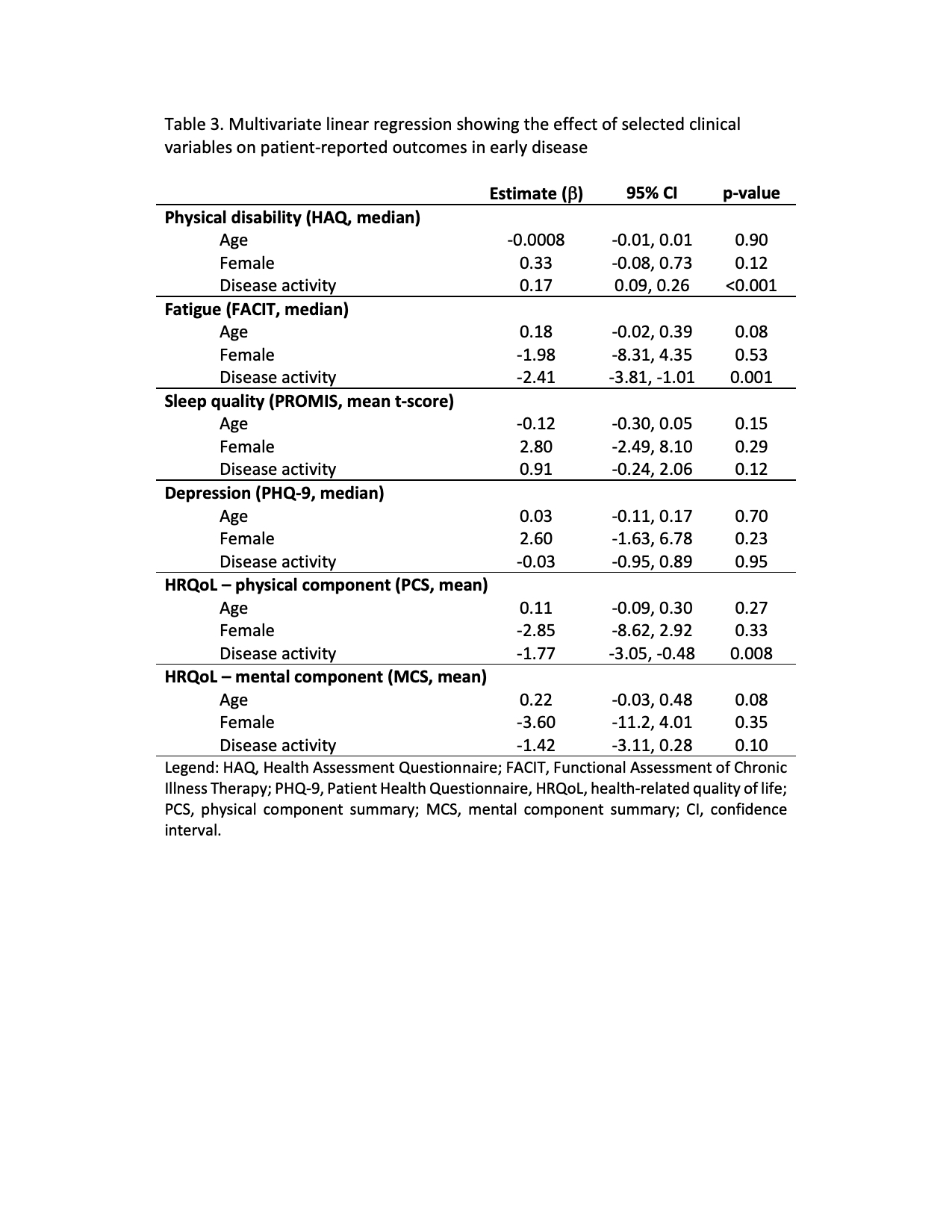
PRO results are presented in Table 2. Median (IQR) HAQ score was 1 (0.3-1.6) indicating moderate disability. Median (IQR) FACIT scores was 28 (19-40). Mean (SD) PROMIS score was 57 (10), indicating substantially worse sleep quality compared with the general population. Median (IQR) PHQ-9 score was 10 (6-16). The mean (SD) SF-36 physical and mental component summary scores were 1.5 SD (35 (11)) and almost 1 SD (42 (15)) below that of the general population, respectively. Multivariate linear regression analyses (Table 3) showed a statistically significant association between disease activity and worse physical functioning measured with the HAQ (β 0.17, 95%CI 0.09, 0.26), more fatigue measured with the FACIT (β -2.41, 95%CI -3.81, -1.01) and impaired physical HRQoL measured with the SF-36 PCS (β -1.77, 95%CI -3.05, -0.48).
Conclusion: Early AIM subjects feel and function poorly. Impairments in PROs for which standards exist, in particular function, sleep quality and HRQoL, are large, in some cases exceeding 1 SD. There is a need to standardize fatigue and depressive measures to better understand those results. Further research into correlates of and trajectories in PROs in AIM are urgently needed.
To cite this abstract in AMA style:
Leclair V, Thombs B, Wang M, Vinet E, Albert A, Hudson M. Patient-reported Outcomes in Early Autoimmune Inflammatory Myopathies [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/patient-reported-outcomes-in-early-autoimmune-inflammatory-myopathies/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-reported-outcomes-in-early-autoimmune-inflammatory-myopathies/