Session Information
Date: Sunday, November 8, 2020
Title: Epidemiology & Public Health Poster III: Inflammatory Rheumatic Disease
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The objective of the current study was to examine the change in prescribing patterns for older adults with RA over a 20 year period using a validated health administrative database. Specifically we wished to determine if the anticipated changes in prescribing over 2 decades had occurred in the broader population of RA patients and, in particular, if the use of corticosteroids fell over this time.
Methods: This was a secondary analysis of health administrative data using a previously validated dataset and case definition for RA. Cases were matched 1:4 by age and sex to controls within a population of approximately 1 million inhabitants with access to universal health care. Longitudinal data for incident and prevalent RA cases were studied between 1997 and 2017. Statistical analyses included descriptive statistics and linear regression.
Results: There were 8240 RA cases (all ≥ 65 years) with a mean (SD) age 72.2 (7.5) years and 70.6% were female. Over 20 years, annual utilization of coxibs in prevalent RA cases fell with a concomitant increase in disease modifying anti-rheumatic drugs (DMARDs) and biologics. Over the same period corticosteroid use was largely unchanged. Approximately one third of patients had at least one annual prescription for corticosteroid, most frequently prednisone. The mean annual dose showed a modest reduction and the duration of utilization in each year shortened. Rheumatologists prescribed corticosteroids less frequently and in lower doses than other physician groups. For incident RA cases there was a significant fall in annual prescribed dose of prednisone by rheumatologists over time.
Conclusion: In older adults with RA the utilization of DMARDs and biologics has increased over the past 20 years. However, the use of corticosteroids has persisted. Renewed efforts are required to minimize their use in the long-term pharmacological management of RA.
 Figure 1: Annual utilization of coxibs, corticosteroids, disease modifying anti-rheumatic drugs (DMARDs) and biologics over 20 years as indicated by the proportion of RA cases and controls who received one or more prescriptions per year.
Figure 1: Annual utilization of coxibs, corticosteroids, disease modifying anti-rheumatic drugs (DMARDs) and biologics over 20 years as indicated by the proportion of RA cases and controls who received one or more prescriptions per year.
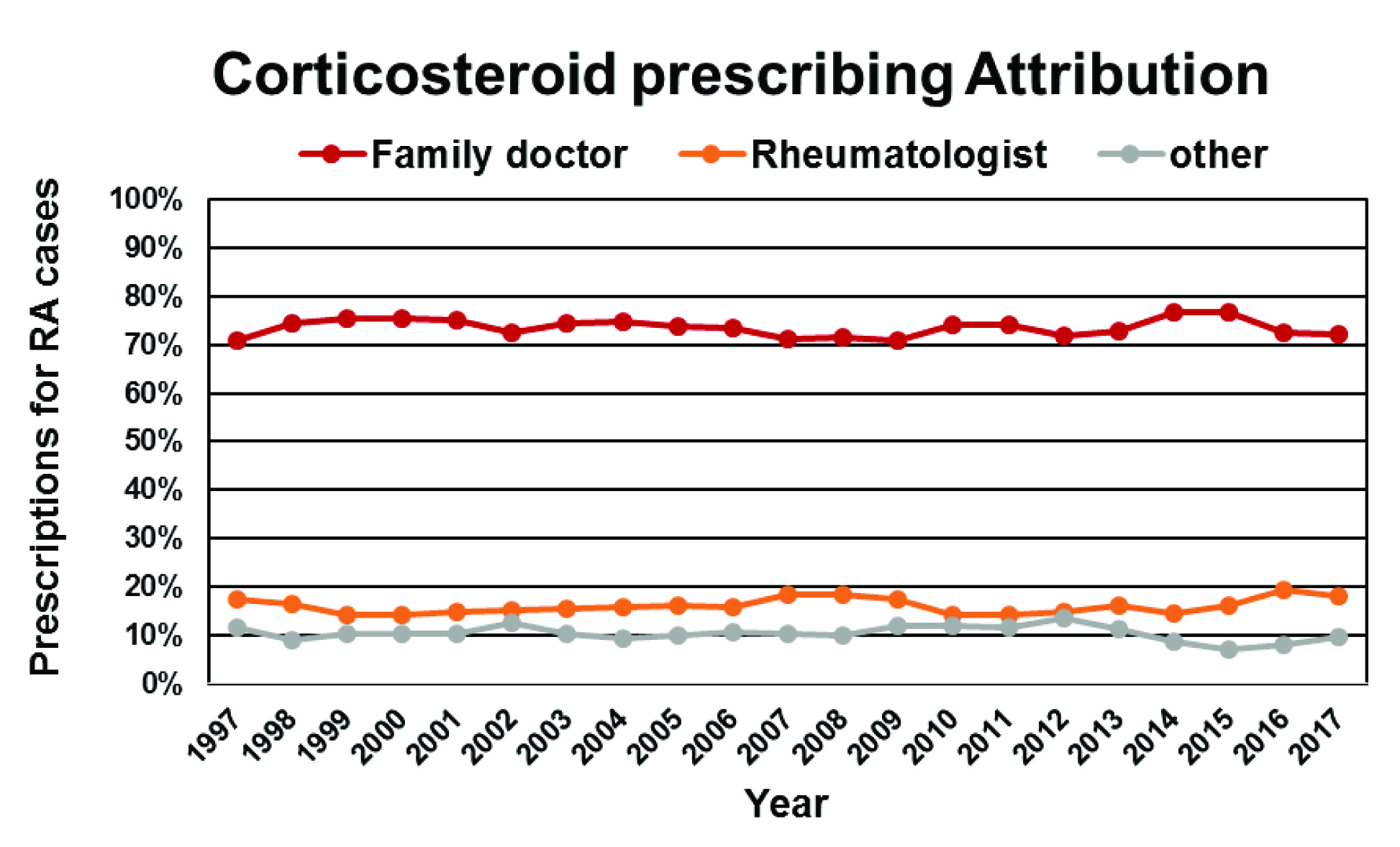 Figure 2: The annual proportion of total corticosteroid prescriptions for RA cases provided by family physicians and non-family physicians over 20 years.
Figure 2: The annual proportion of total corticosteroid prescriptions for RA cases provided by family physicians and non-family physicians over 20 years.
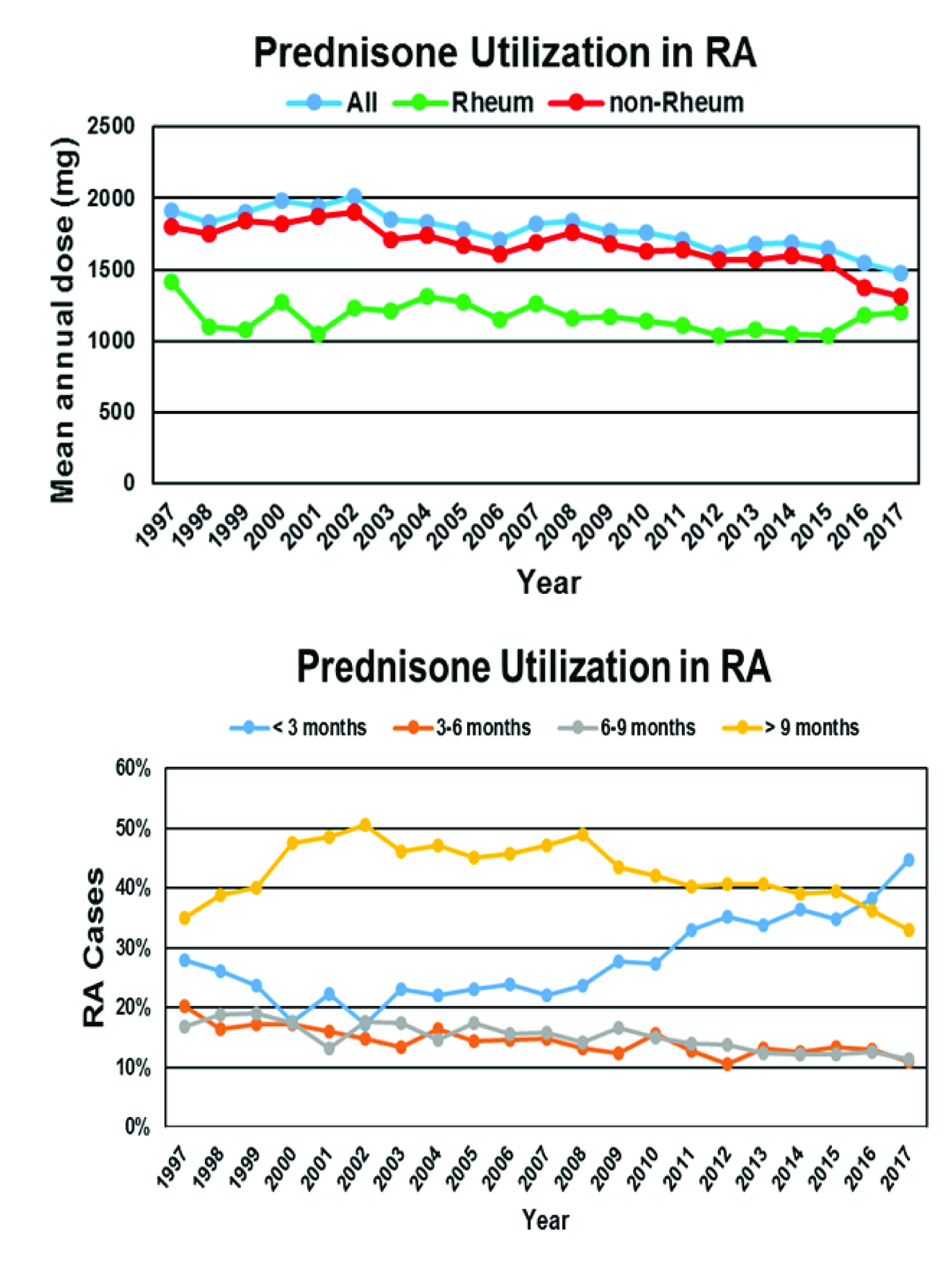 Figure 3: The change in annual utilization of prednisone in RA cases over 20 years. Top panel: change in mean annual dose of prednisone in RA cases and the attribution of prescriptions to rheumatologists (Rheum) and other physician groups (non-Rheum). Some patients received prescriptions from both rheumatologists and other physicians in the same year. Bottom panel: change in the annual duration of exposure to prednisone in RA cases as assessed by one or more prescriptions in each 3 month interval.
Figure 3: The change in annual utilization of prednisone in RA cases over 20 years. Top panel: change in mean annual dose of prednisone in RA cases and the attribution of prescriptions to rheumatologists (Rheum) and other physician groups (non-Rheum). Some patients received prescriptions from both rheumatologists and other physicians in the same year. Bottom panel: change in the annual duration of exposure to prednisone in RA cases as assessed by one or more prescriptions in each 3 month interval.
To cite this abstract in AMA style:
Hanly J, Lethbridge L. Disease Modifying Anti-rheumatic Drugs, Biologics and Corticosteroid Use in Older Patients with Rheumatoid Arthritis over 20 Years [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/disease-modifying-anti-rheumatic-drugs-biologics-and-corticosteroid-use-in-older-patients-with-rheumatoid-arthritis-over-20-years/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/disease-modifying-anti-rheumatic-drugs-biologics-and-corticosteroid-use-in-older-patients-with-rheumatoid-arthritis-over-20-years/
