Session Information
Date: Sunday, November 8, 2020
Title: Epidemiology & Public Health Poster III: Inflammatory Rheumatic Disease
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The involvement of female hormones in the pathogenesis of Rheumatoid Arthritis (RA) is supported by numerous observations: a female predominance, an increased incidence in the post-partum, and around the age of menopause. In the literature, findings on the association between reproductive and hormonal factors, taken individually, and RA are conflicting. Our objectives were to assess the relationships between lifetime durations/level of female hormonal exposures and the risk of RA.
Methods: E3N is an ongoing French prospective cohort of 98,995 women since 1990 aged 40-65 years at enrolment. Validation of RA cases among the cohort has been previously published [Nguyen et al. BMJ Open 2019]. Lifetime female hormonal exposures were defined as follows:
– Reproductive span (in years) = duration from menarche to menopause
– Total ovulatory years (in years, time-dependent) = Reproductive span – (number of full-term pregnancies x 0.75 + number of miscarriages x 0.25 + total duration of breast feeding + total duration of oral contraception)
– Lifetime hormonal exposure (in years, time-dependent) = Reproductive span + total duration of menopausal hormonal therapy
– Composite Estrogen Score (CES, range = 0–5, time-dependent), calculated by point assignment for early menarche (≤10 years), high parity ( >3 pregnancies), history of hysterectomy, use of hormone therapy (oral contraception and/or menopausal hormonal therapy, ever) and late menopause (≥53 years).
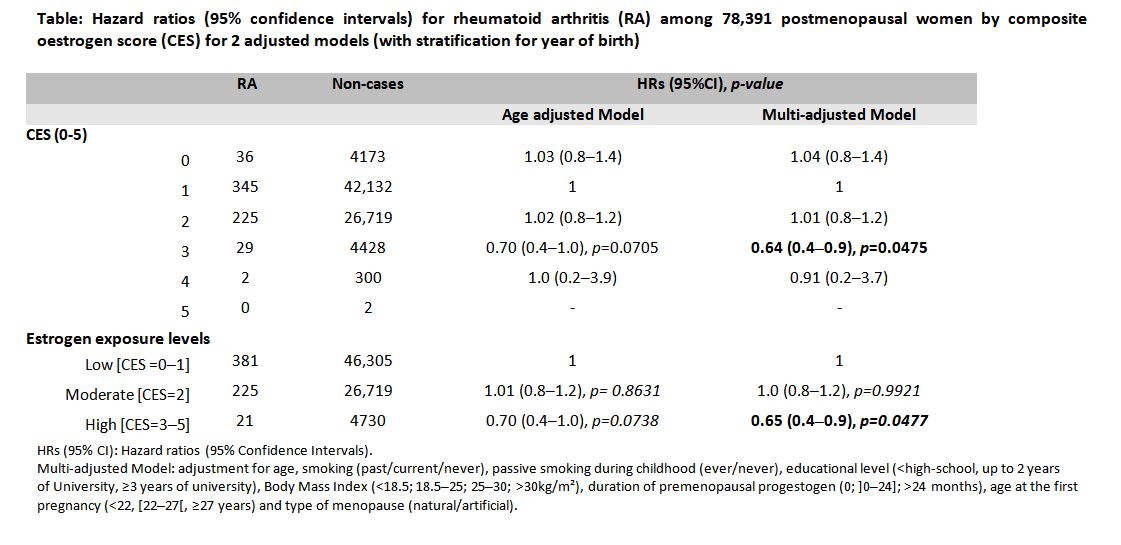
Hazard ratios (HRs) and 95% confidence intervals (CIs) for the risk of incident RA were estimated using Cox proportional hazards regression models with age as the time scale.
Models were adjusted for age (age-adjusted model) and additionally for smoking, passive smoking during childhood, educational level, body mass index , duration of premenopausal progestogen, age at the first pregnancy and type of menopause (multi-adjusted model).
Results: A total of 637 incident RA cases occurred among 78,391 post-menopausal women with a total of 1,864,915 women-years from baseline.
Reproductive span, total ovulatory years and lifetime hormonal exposure were not significantly associated with incident RA in postmenopausal women in age adjusted models (p for trend=0.2479, p for trend=0.4343, p for trend=0.9216 , respectively).
In multivariable-adjusted Cox regression models, high level of estrogen exposure (CES=3-5) was inversely associated with the risk of RA in post-menopausal women: HR=0.65 (95%CI 0.4–0.9), p=0.04, taking low level (CES=0-1) as reference (Table).
Interestingly, in a recent publication, high level of CES was associated with a reduced risk of primary Sjögren, but not cumulative menstrual cycling (reproductive span minus time to pregnant) [McCoy et al. Arthritis Care Res 2019]. RA and primary Sjögren share a marked female predominance with a peak onset around menopause and the participation of B lymphocytes in this physiopathology.
Conclusion: In E3N cohort, a high CES which reflects lifetime exposure to estrogen was associated with a decreased risk of RA in postmenopausal women.
To cite this abstract in AMA style:
Salliot C, Nguyen Y, Gelot A, Mariette X, Boutron-Ruault M, Seror R. Post-menopausal Rheumatoid Arthritis Is Inversely Associated with Lifetime High Level of Estrogen Exposure in the French E3N Cohort [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/post-menopausal-rheumatoid-arthritis-is-inversely-associated-with-lifetime-high-level-of-estrogen-exposure-in-the-french-e3n-cohort/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/post-menopausal-rheumatoid-arthritis-is-inversely-associated-with-lifetime-high-level-of-estrogen-exposure-in-the-french-e3n-cohort/