Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: The management of gout is heterogeneous across specialties and clinical settings. Gout has been demonstrated to be one of the most poorly managed conditions in healthcare. Identifying the gaps in gout management can help in focusing research to identify novel interventions or models of care that may enhance gout management and improve clinical outcomes. The purpose of this study was to assess current practices and perspectives in gout management regarding the etiology of substandard gout management amongst rheumatologists internationally.
Methods: A cross-section non-compensated survey of rheumatologists across the world was distributed to practicing rheumatologist members of the ACR and Gout, Hyperuricemia and Crystal-Associated Disease Network (G-CAN) using a 28-item questionnaire designed to evaluate current clinical practice of gout management and to assess barriers to optimal gout management. This was an anonymous internet survey open from 05/1/2020 to 05/14/2020.
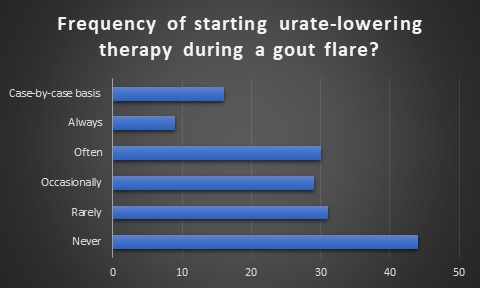
Results: The survey had a response rate of 8.5% (161/1900) with 60.2% being male. The age groups of respondents was evenly distributed from under 35 to great than 66 years. Majority of respondents had greater than 10 years of clinical practice (65.6%). 70.2% were academic rheumatologists. 71.4% practiced in the United States. 31.3% of respondents were G-CAN members. The mean number of gout cases seen per month by respondents was 21.3 with a median of 10. The overall survey results were concordant with the 2020 ACR guidelines. Two areas of discordance with these guidelines were identified. 1) 64.6% of respondents preferred not to start ULT during an acute flare. (Figure 1) 2) 59.6% of respondents reported “never” or “rarely considered” HLA-B*58:01 genetic testing.
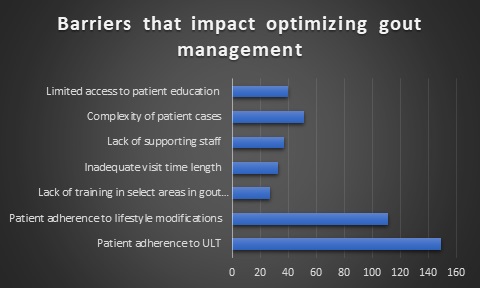
Regarding improving gout management, respondents identified patient compliance with ULT (94.3%) and lifestyle changes (70.3%) as the predominant factors(Figure 2). From the perspective of healthcare improvement of gout care, physician education, involvement of other members of the healthcare team, and better access to patient education tools, were all identified as areas of potential improvement(Figure 3).
Conclusion: Despite the modest response rate, our study highlights a variety of targets to improve care of patients with gout. Education for physicians regarding the potential benefits of initiation of ULT during an acute flare appears to be a straightforward concept to address. The polled rheumatologist’s current gout management practices per our survey results are consistent with the 2020 ACR gout management guidelines. This consistency in guideline directed care of gout patients provides evidence for a rheumatologist directed gout care team.
We identified two main areas of focus for future studies based on our results: 1) Methods of assisting patients with adherence to ULT and lifestyle changes 2) Enhanced inclusivity of the entire healthcare team in treatment of gout patients. Programs targeting these gaps may lead to better management of gout by the healthcare system and aid in reducing the prevalence of this burdensome disease.
To cite this abstract in AMA style:
Gavin J, KC Y, Dombrosky E, Shah N, Roman Y. Surveying Practicing Rheumatologists Regarding Gout Management and Barriers in Gout Care [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/surveying-practicing-rheumatologists-regarding-gout-management-and-barriers-in-gout-care/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/surveying-practicing-rheumatologists-regarding-gout-management-and-barriers-in-gout-care/