Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Many patients with rheumatic diseases are at increased risk of infection, including invasive pneumococcal infection, due to both disease-related abnormalities of the immune system as well as the use of immunomodulatory medications. The Centers for Disease Control and Prevention recommends that people with immunocompromising conditions receive vaccination with both a pneumococcal conjugate vaccine (PCV-13), and pneumococcal polysaccharide vaccine (PPSV-23). However, significant confusion persists in rheumatology clinics regarding pneumococcal vaccine indications and algorithms for administering the vaccine. Furthermore, multiple competing demands in clinic often leave inadequate time to discuss indicated vaccinations with patients. The aim of our quality improvement initiative was to improve the percentage of patients who are up to date on pneumococcal vaccines in an academic county hospital rheumatology clinic from 33% to 53% for PCV-13 and from 49% to 70% for PPSV-23 from January 2019 to January 2020.
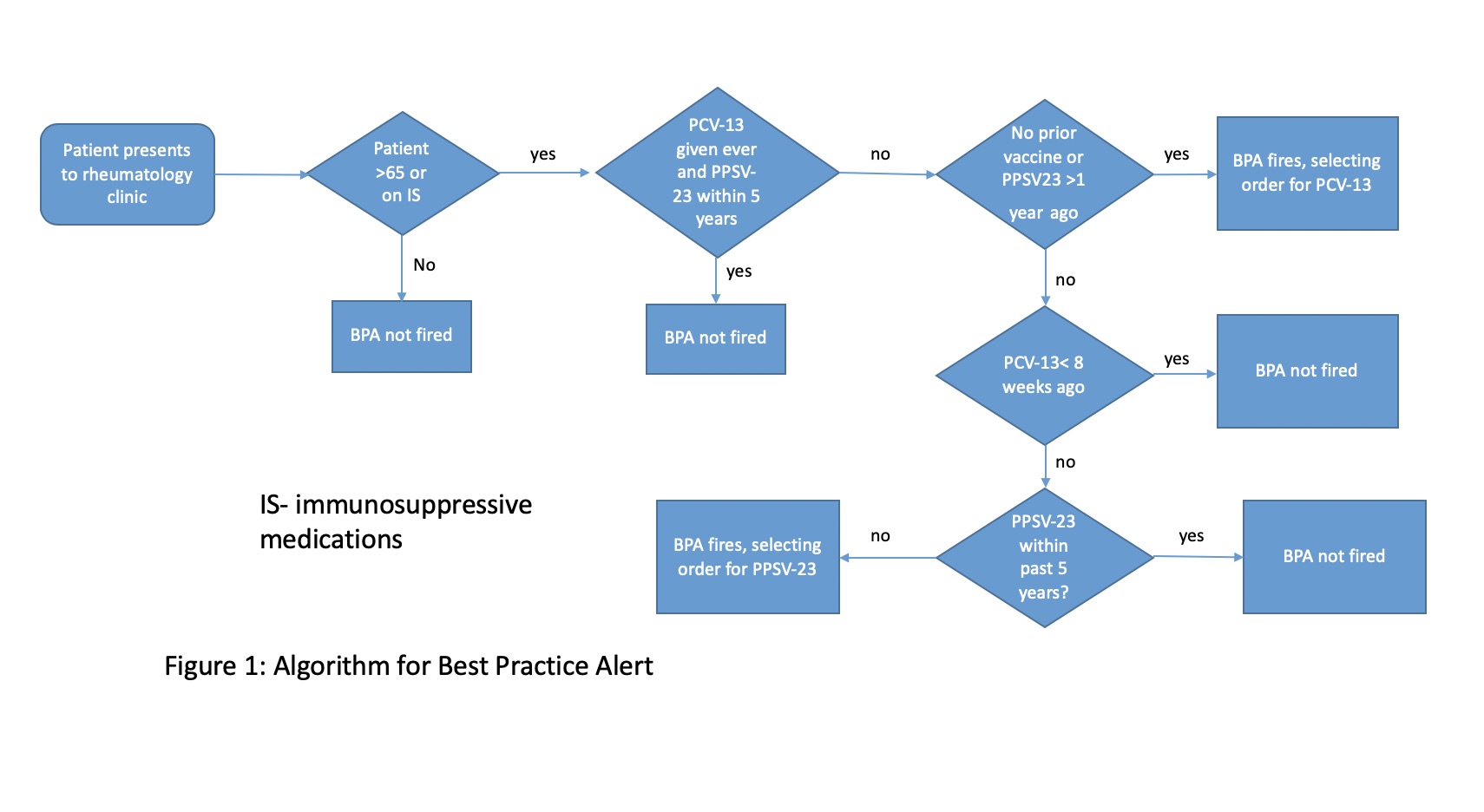
Methods: We created a Best Practice Alert (BPA) in our electronic medical record that would alert the provider when a patient is due for either a PCV-13 or PPSV-23 vaccine (Figure 1). The BPA opens an order set with the appropriate vaccine preselected. The provider then has to sign the vaccine order and a nurse will administer it as part of the checkout process. A comprehensive list of immunosuppressive medications was given to the hospital information technology department to incorporate into the BPA algorithm. The BPA went live in December 2019. In order to have consistent results, we reviewed 50 patient charts from the first week of January 2019 and 50 patient charts from the first week of January 2020. Patients seen by the authors, who refused vaccination, or who did not have an indication for pneumococcal vaccination were excluded. Patients who had received one vaccination but were not yet due for the other were counted as up to date on vaccination status.
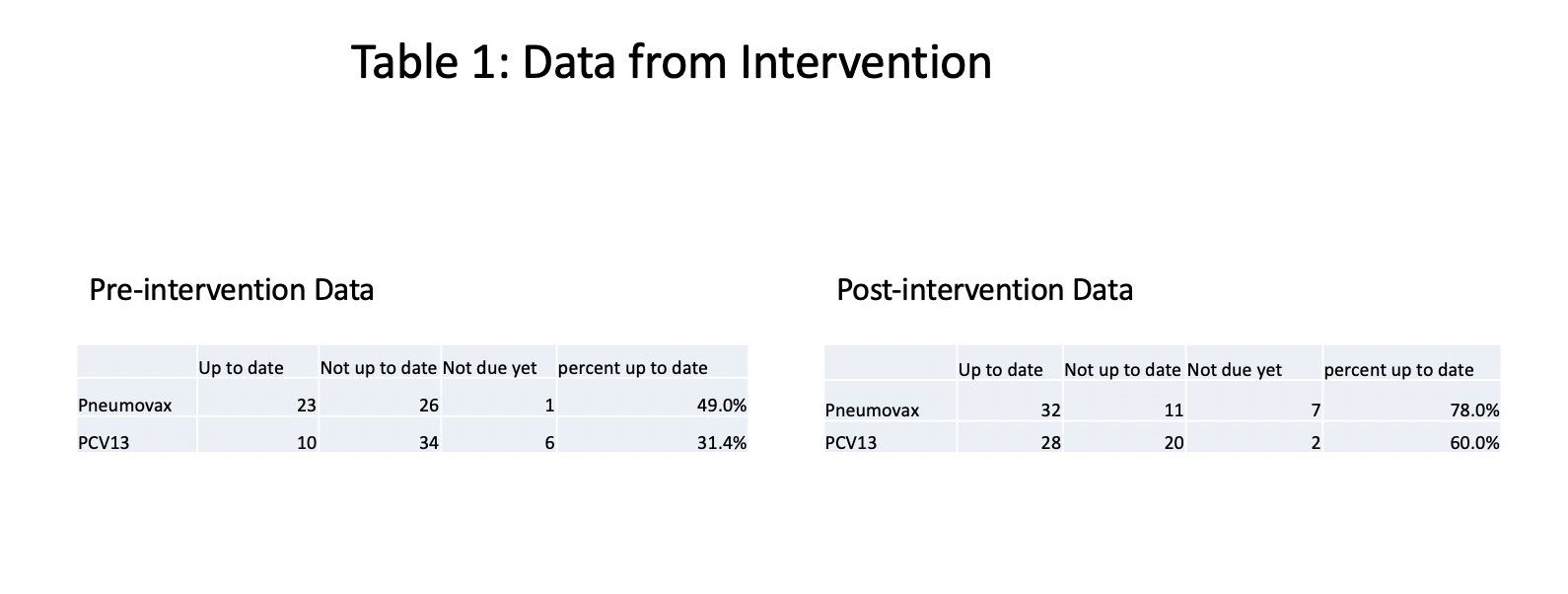
Results: Of 50 patient charts reviewed pre-intervention from January 2019, 31% were up to date on PCV-13 and 49% were up to date on PPSV-23 vaccination. In January 2020, post-intervention, 60% were up to date on PCV-13 and 78% of patients were up to date on PPSV-23, exceeding our goal. The vast majority of patients were on at least one immunosuppressive medication (Tables 1 and 2).
Conclusion: Patients with rheumatic conditions have an indication for pneumococcal vaccination, but are not always vaccinated. This quality improvement project utilizes the medical record to remind providers to discuss appropriate pneumococcal vaccination based on an algorithm and rapidly order the vaccine if the patient agrees. We have shown in our clinic that BPAs are effective at increasing pneumococcal vaccination rates in our outpatient rheumatology clinic. Further data will be needed to assess sustainability of the intervention.
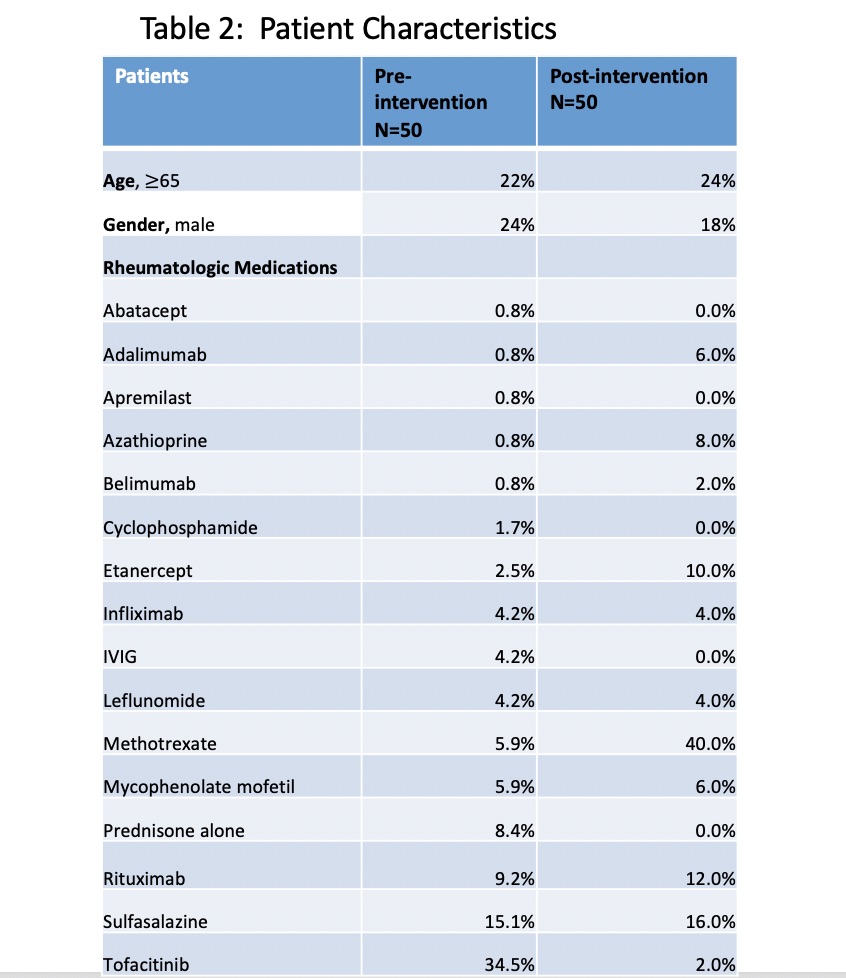 Table 2- Patient characteristics
Table 2- Patient characteristics
To cite this abstract in AMA style:
Bacalao M, Reddy S, Syed N. Increasing the Rate of Pneumococcal Vaccination in an Academic Rheumatology Outpatient Clinic [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/increasing-the-rate-of-pneumococcal-vaccination-in-an-academic-rheumatology-outpatient-clinic/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increasing-the-rate-of-pneumococcal-vaccination-in-an-academic-rheumatology-outpatient-clinic/