Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Biologic disease-modifying antirheumatic drug (bDMARD) therapies are commonly prescribed for rheumatoid arthritis (RA) treatment. However, their high out-of-pocket (OOP) cost may limit patient access to therapy. While insurance typically covers bDMARDS, they often require cost-sharing. Prior studies have shown that cost-sharing can have negative consequences, such as nonadherence and increased use of medical services. However, no study has examined adherence changes by drug class across OOP cost ranges in the commercial population. The purpose of this study is to assess the impact of patient OOP cost range, drug class and referral source on adherence in patients with RA.
Methods: This is a retrospective cohort study of RA patients insured by a large commercial health plan in the United States who reported a first RA drug fill for (medical or pharmacy benefit) from March 1, 2018, to February 28, 2019 (index fill), from a single specialty pharmacy. Demographic characteristics, OOP cost, drug class and referral source were obtained from the specialty pharmacy’s dispense data. We defined a direct referral as any incoming referral from a prescriber, another specialty pharmacy, a payor or a patient. We defined a hub referral as a referral from the manufacturer. All other referrals were included in the “other” category. Medication adherence was calculated using the medication possession ratio (MPR). MPR was defined as the sum of the days’ supply for all fills of RA drugs during a year after the index fill, divided by 365. A generalized linear model (GLM) was used to estimate predictors of adherence.
Results: The study included 16,200 patients, the majority were female (74.7%) and the mean age was 50.8 years (SD = 12.0). The average copay per day supply was $0.89 (SD = $5.79). Most (81.4%) patients used a coupon at least once to pay for their medication. Patients in the lowest copay category, compared to the other copay categories, were more likely to use a coupon (83.2%) to pay for their medication (p < 0.001). After adjusting for the variables in the model, MPR decreased as OOP cost increased. Above an OOP cost of $181 per month, MPR decreased significantly (p =0.0004). MPR was significantly different by drug class (p < 0.01), IL6 = 59.9%, TCB = 64.2%, TNF = 66.8% and JAK = 66.8%. Patients who received a direct referral had a significantly higher MPR (66.5%) compared to patients who received a referral from an “other” source (61.1%) (p < 0.0001).
Conclusion: This study suggests that as member OOP costs increase adherence decreases and adherence differs by drug class and referral source. Source of referral and an appropriate formulary and patient copayment structure must be considered when assessing adherence.
 Table 1. Demographic Characteristics (N=16,200)
Table 1. Demographic Characteristics (N=16,200)
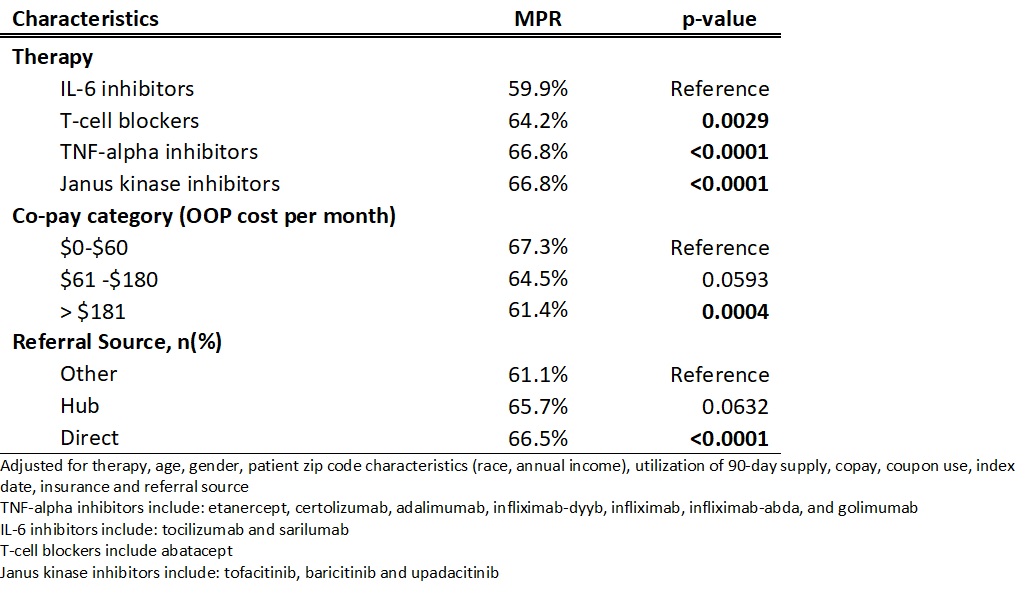 Table 2. Adjusted Generalized Linear Model
Table 2. Adjusted Generalized Linear Model
To cite this abstract in AMA style:
Cozzi G, Kyrychenko P, Hamburger M, Avalos-Reyes E. Risk Factors of Nonadherence in New Rheumatoid Arthritis Patients [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/risk-factors-of-nonadherence-in-new-rheumatoid-arthritis-patients/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-of-nonadherence-in-new-rheumatoid-arthritis-patients/
