Session Information
Session Type: Abstract Session
Session Time: 10:00AM-10:50AM
Background/Purpose: In spite of the increasing burden of rheumatic diseases in the United States, many patients have limited access to rheumatologists. As a result, internists provide much of the care for these patients. However, the current state of rheumatology education for internal medicine (IM) residents is inadequate. No national rheumatology curriculum exists for IM residents. At the University of California San Francisco (UCSF), 20% of IM residents report dissatisfaction with their clinical and didactic experience in rheumatology and in-training exam scores in rheumatology are consistently in the bottom 3 specialties. The purpose of this study was to determine expert consensus on the most important topics to include in a curriculum for UCSF IM residents.
Methods: We conducted a modified, 2-round Delphi process to develop consensus on rheumatology topics that all graduating IM residents should know. Through review of the literature for common diagnoses and the ABIM Blueprint in rheumatology, we generated an initial list of 78 topics. We surveyed 50 expert faculty educators from general internal medicine, hospital medicine, and rheumatology, and asked them to rate each topic’s importance using a 4-point Likert scale (0 = absolutely do not include, 1 = not very important, 2 = kind of important, 3 = important, 4 = very important). We considered a content validity index (the percentage of respondents who rated the topic as ≥3 in Round 2) of at least 80% as our definition for having reached consensus.
Results: 35 of 50 (70%) completed Round 1 of the survey, and 27 of 35 (77%) completed Round 2 (total response rate 54%). In Round 1, 63.6% of topics were scored as ≥3, with a significant difference in scoring between rheumatologists and general medicine faculty (56.2% vs. 69%, p=0.009). 30 of 78 topics met our consensus definition (scored as ≥3 by at least 80% of respondents), with 21 of 78 meeting consensus by rheumatologists compared with 31 of 78 by general internists (p=0.09). 8 additional topics proposed by participants in Round 1 were included in Round 2. After Round 2, 35 of 86 topics met the consensus definition, with rheumatologists reaching consensus on fewer topics than general internists (33.7% versus 44.2% of topics, p=0.16). 74.2% of the topics meeting consensus addressed clinical features and/or diagnostics of rheumatologic conditions, while the remainder focused on treatment.
Conclusion: The Delphi consensus method was used to determine which topics should be included in a rheumatology curriculum for IM residents. This process can be used as a blueprint for development of curricula in other medicine specialties in our and other residency programs. Interestingly, rheumatologists considered more topics to be of lower importance to include in a curriculum for IM residents compared with ratings by general internists. The potential differences in opinion between rheumatologists and general internists highlights the need to include both specialists and general medicine physicians in developing subspecialty curricula.
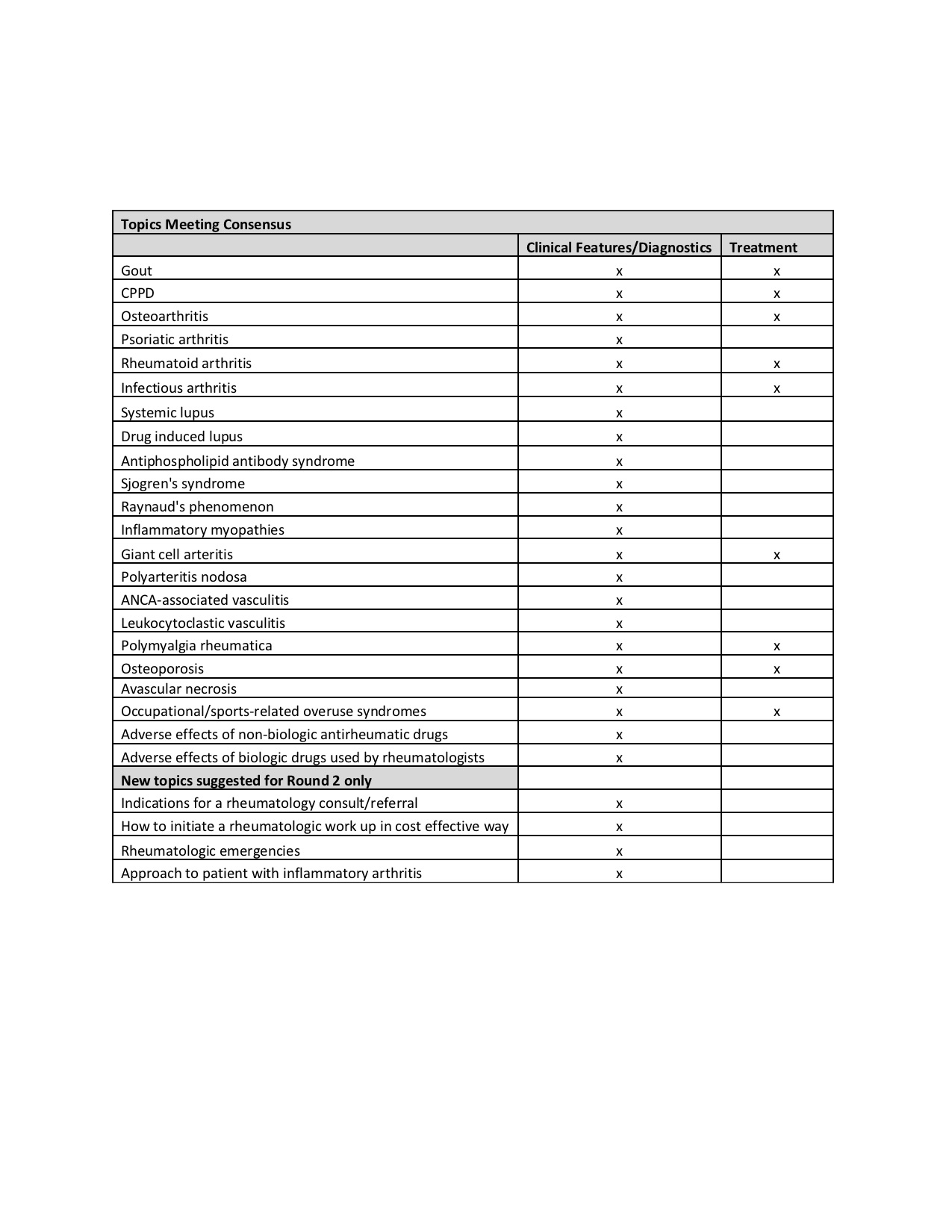 Table 1. Topics meeting consensus after Round 2 of Delphi process categorized as either clinical features/diagnostics or treatment of specific rheumatologic condition
Table 1. Topics meeting consensus after Round 2 of Delphi process categorized as either clinical features/diagnostics or treatment of specific rheumatologic condition
To cite this abstract in AMA style:
Goglin S, Babik J. Using Consensus Building to Guide Rheumatology Curriculum Development for Internal Medicine Residents [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/using-consensus-building-to-guide-rheumatology-curriculum-development-for-internal-medicine-residents/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/using-consensus-building-to-guide-rheumatology-curriculum-development-for-internal-medicine-residents/
