Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Aortitis was previously regarded as a rare form of large vessel vasculitis (LVV), but is now increasingly being recognised. It may occur in the context of primary systemic vasculitis, as a part of systemic autoimmune disease or in isolation. Positron emission tomography (PET) has facilitated the diagnosis of LVV which is often a challenge as the presenting clinical features are often nonspecific. The outcome and optimal management remain uncertain; EULAR 2018 recommendations on LVV have helped to address some of these issues [EULAR 2018 guidelines (Hellmich B, et al. Ann Rheum Dis 2020;79:19–30)]
We aimed to assess the presenting features, time to diagnosis, imaging methods utilized, treatment and complications in a cohort of patients with isolated aortitis.
Methods: We identified patients diagnosed with isolated aortitis presenting at our centre over the last 10-years. Patients were identified using a specifically designed database, which prospectively phenotyped all patients attending a single rheumatology department. Their medical notes were retrospectively reviewed using the electronic patient record system.
Results: We identified 63 patients who had been diagnosed with isolated aortitis (IA) over the last 10 years; 5 were excluded due to incomplete data.
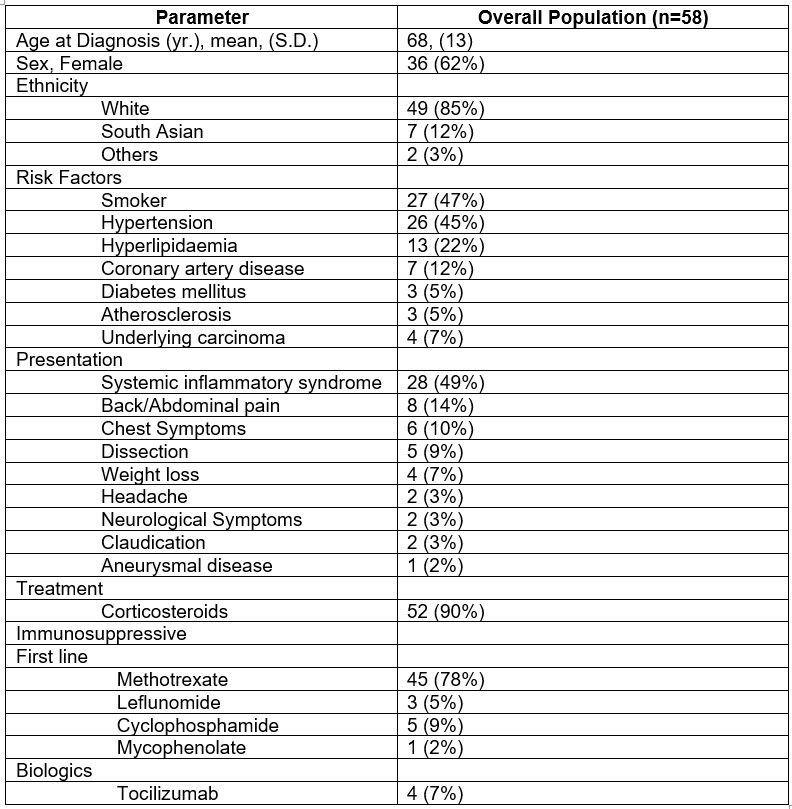
Demographic data and main results are presented in Table 1. The median age at diagnosis of aortitis was 68 years (range 32 – 88); 36 (62%) were females. The median duration of symptoms was 7 months (range 2-120). The commonest presenting feature was systemic inflammatory syndrome in 28 patients (49%) followed by back/abdominal pain in 8, chest symptoms in 6 and weight loss in 4. Acute presentation with dissection/aneurysm was seen in 6 patients who also had histological confirmation of aortitis.
Patients had elevated inflammatory markers (median CRP 81 [range16-249]; median ESR 79 [range 11-139]) at presentation. 43 patients (74%) were diagnosed on PET CT with aortitis, 12 (21%) on CT angiogram aorta (CTA) and 3 (5%) on CT chest/full body performed to rule out other diagnoses. Follow up imaging included MRA in 60, CTA in 56 and PET CT in 30 patients.
Prednisolone and disease modifying anti-rheumatic drugs (DMARDs) were used in the majority of patients (90% and 93% respectively), with methotrexate being the commonest DMARD. Cyclophosphamide was used in 11 patients and 4 patients received tocilizumab.
The median duration of follow up was 3 years (range 0.30 – 10). 17 patients developed vascular complications, including aneurysms (8 patients), vascular stenosis/ischaemic complications (9 patients) with 4 patients requiring subsequent vascular/surgical interventions.
Drug free remission was achieved in 13 (23%) patients and they remain in remission whilst off treatment for a median duration of 11 months (range 2-40). 4 patients died during follow up, 3 due to sepsis and 1 to unknown cause.
Conclusion: We have reviewed the clinical features, treatment and complications of a cohort of patients with isolated aortitis. Diagnostic delay remains an issue, highlighting the need for increasing awareness of this condition. Vascular complications are high in this group, despite aggressive immunosuppression and only a minority achieve sustained drug free remission.
To cite this abstract in AMA style:
Ahmad N, Verdiyeva A, Luqmani R, Dubey S. Isolated Aortitis: Single Centre Experience of Clinical Spectrum and Management [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/isolated-aortitis-single-centre-experience-of-clinical-spectrum-and-management/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/isolated-aortitis-single-centre-experience-of-clinical-spectrum-and-management/