Session Information
Date: Friday, November 6, 2020
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Psoriatic arthritis (PsA), a systemic inflammatory disease, occurs in about 25% of patients with psoriasis (PsO). At present, there are no biomarkers that reliably identify patients with PsO who will go on to develop PsA. In addition to peripheral and axial arthritis, enthesitis is common in PsA. Oxylipins are biological lipids that have been implicated in various pathological processes, including inflammation. We previously found that certain oxylipins correlated with joint disease and skin disease in a cohort with PsA patients. Here, we compare the oxylipin profile in two different cohorts of PsO patients without joint disease and PsA patients.
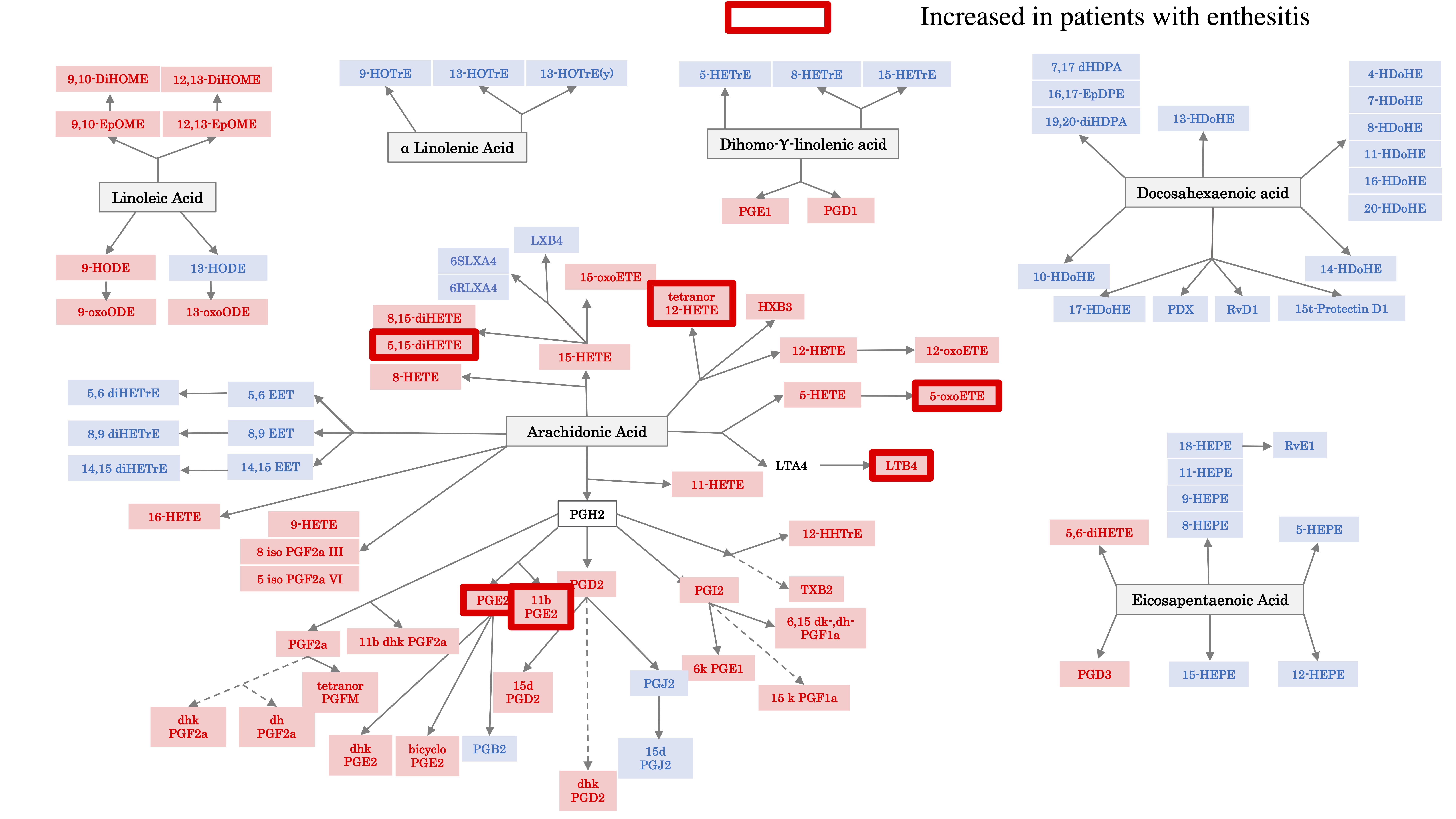
Methods: Patients with PsA and PsO, diagnosed based on the CASPAR criteria were recruited from the Rheumatology Outpatient Clinic at the University of Rochester, NY. A thorough clinical examination was performed, including enthesitis (using Leeds index). Patients completed a health assessment questionnaire. DAS (disease activity score) 44, Psoriasis Area and Severity Index (PASI) and body surface area (BSA) of psoriasis were also calculated. Serum oxylipins were determined by Mass Spectrometry and were classified into groups according to their precursor: arachidonic acid (AA), linoleic acid (LA), a-Linolenic acid, Docosahexaenoic acid (DHA), eicosapentaenoic acid (EPA) and Dihomo-g-linolenic acid. Data were analyzed using R version 3.6.1.
Results: Sera from 20 PsO patients were analyzed (average age 51.95 (10.83), 55% males, average body mass index BMI; 33.73 (6.84)). The average PASI was of 3.87 (4.25) and there was an average BSA of 4.5 (4.77). PsO patients were classified in 2 groups, based on the PASI. The group with higher PASI score ( >2.5) had significantly lower serum concentrations of pro-inflammatory oxylipins, most of them being derived from AA. 19 PsA patients were analyzed (average age 60.5 years old (11.41), 63.15% males, with an average BMI of 31.96 (5.64)). The average number of TJC was 9.38 (10.41) and of SJC 3.77 (4.23). 63.15% patients had enthesitis (average of 2.21 (3.08)) and psoriasis (average PASI 3.02 (5.09)). Oxylipins profiling in the PsA patients with higher PASI score ( >2.5) also had lower AA-derived oxylipins compared to PASI ≤ 2.5 . Oxylipin profiling did not associate with the number of SJC nor TJC. Yet, interestingly, several AA-derived oxylipins (8,15 di-HETE, 5-oxoETE, PGE2, 11bPGE2, 5-oxoETE, LTB4) were significantly associated with enthesitis. PsA patients with enthesitis had higher concentrations of oxylipins compared to PsA patients without enthesitis (Figure 1).
Conclusion: The AA-derived proinflammatory oxylipins were lower in both PsO and PsA patients with higher skin scores. Joint disease activity didn’t have an effect on the concentrations of oxylipins. Yet, enthesitis was associated with an increase of AA derived pro-inflammatory oxylipins. Further studies are needed to determine whether oxylipin profiling can be a good biomarker of enthesitis in PsO patients.
To cite this abstract in AMA style:
Coras R, Kavanaugh A, Kluzniak A, Holt D, Weilgosz A, Quehenberger O, Ritchlin C, Guma M. Oxylipin Profile Is Associated with Skin Disease and Enthesitis in Psoriatic Disease [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/oxylipin-profile-is-associated-with-skin-disease-and-enthesitis-in-psoriatic-disease/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/oxylipin-profile-is-associated-with-skin-disease-and-enthesitis-in-psoriatic-disease/