Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Inappropriate sensing of nucleic acids leading to enhanced type I interferon (IFN) induction is a hallmark of SLE, contributing to breakdown of immune tolerance and driving pathology. Cytosolic DNA is sensed by cyclic GMP-AMP synthase (cGAS), which synthesizes cyclic GMP-AMP (cGAMP), a potent second messenger that activates STING-dependent type 1 IFN (R Zhou et al., 2019). Recently, the cGAS-STING pathway has been implicated in SLE by the observation that cGAS expression and cGAMP levels were elevated in SLE PBMCs compared to healthy controls (J An et al., 2017). Also, it has emerged that cGAMP can be transported across the cell membrane by SLC19A1, a reduced folate transporter that is found on myeloid cells, leading to direct activation of STING. Interestingly, methotrexate (MTX) is a potent inhibitor of SLC19A1 import of cGAMP in monocytes (RD Luteijn et al., 2019). Here we explore the potential that altered SLC19A1 expression may contribute to increased IFN responses in SLE.
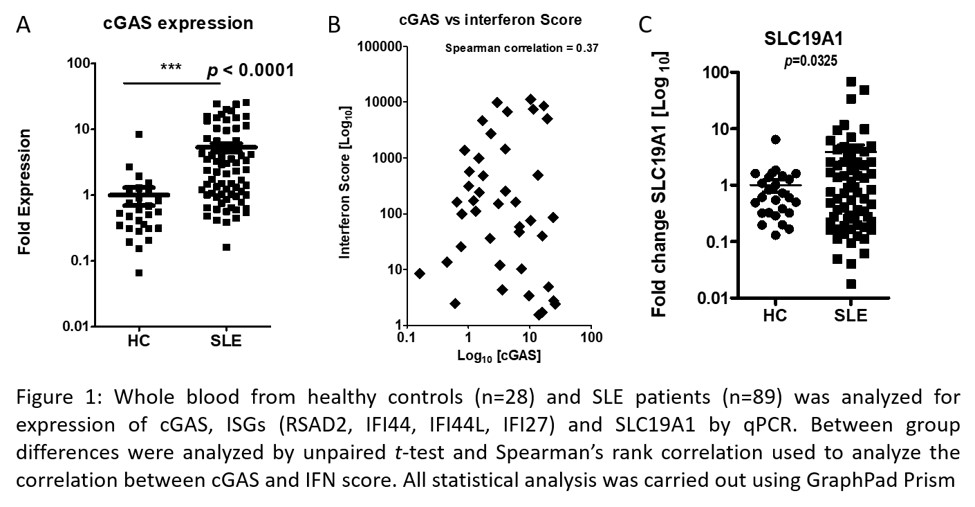
Methods: Peripheral blood samples from SLE patients (meeting ACR classification criteria for SLE) and healthy controls (HC) were collected via a protocol approved by the local institutional review board. Monocytes were isolated from peripheral blood using CD14+ immunomagnetic bead isolation (StemCell Technologies). For gene expression analysis, qPCR analysis was performed using ddCt method, and statistical analyses were performed using GraphPad Prism 5. Four interferon stimulated genes (ISG) RSAD2, IFI44, IFI44L, IFI27 were used to calculate IFN scores, which are associated with increased disease activity in SLE patients (X Feng et al., 2006).
Results: A total of 28 HCs and 89 SLE patients were enrolled in an independent cohort. 95% of the patients were female, with a mean age of 44 (SD ± 13 years). In keeping with cGAS as an ISG, its expression was significantly higher in the peripheral blood of SLE patients compared to HC (p< 0.0001) (figure 1a) and correlated positively with IFN score measured in the same samples (figure 1b). Expression of SLC19A1 was also significantly higher (p=0.0325) in SLE patient blood compared to HC (figure 1c). In examining the level of expression on patient monocytes compared to those from HC, SLC19A1 was found to be increased on the surface of cells as determined by flow cytometry (data not shown). In assessing how methotrexate (MTX) use altered SLC19A1 at the mRNA level, no difference was seen between those taking MTX (32.9%) and those not. Our preliminary data also indicates that cGAMP and type I IFN can also regulate SLC19A1 expression in whole blood but as to whether there are differences between responses in HC and SLE patient cells is currently been assessed.
Conclusion: Increased cGAS expression in SLE patients was consistent with previous reports, in keeping with it being an ISG. Our observation that the cGAMP transporter SLC19A1 is increased is in keeping with the observed elevation of cGAMP levels detected previously in SLE patient serum (J An et al., 2017). This suggests that altered SLC19A1 expression may contribute to enhanced IFNβ expression via direct uptake and activation of STING. Whether enhanced SLC19A1 expression on cells correlates with enhanced cGAMP uptake and STING activation is currently been assessed.
To cite this abstract in AMA style:
Yu J, Tumurkhuu G, Montano E, de los Santos G, Wallace D, Ishimori M, Jefferies C. Expression of the cGAMP Transporter SLC19A1 Is Altered in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/expression-of-the-cgamp-transporter-slc19a1-is-altered-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/expression-of-the-cgamp-transporter-slc19a1-is-altered-in-systemic-lupus-erythematosus/