Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatic diseases are associated with increased systemic bone loss and fracture risk related to chronic inflammation, disease-specific, general and demographic risk factors as well as treatment with glucocorticoids (GC). The purpose of this study was to investigate the prevalence of osteoporosis and fragility fractures in patients with inflammatory rheumatic diseases and to analyze the impact that treatment with GCs, other known risk factors and preventive measures have on bone health in these patients.
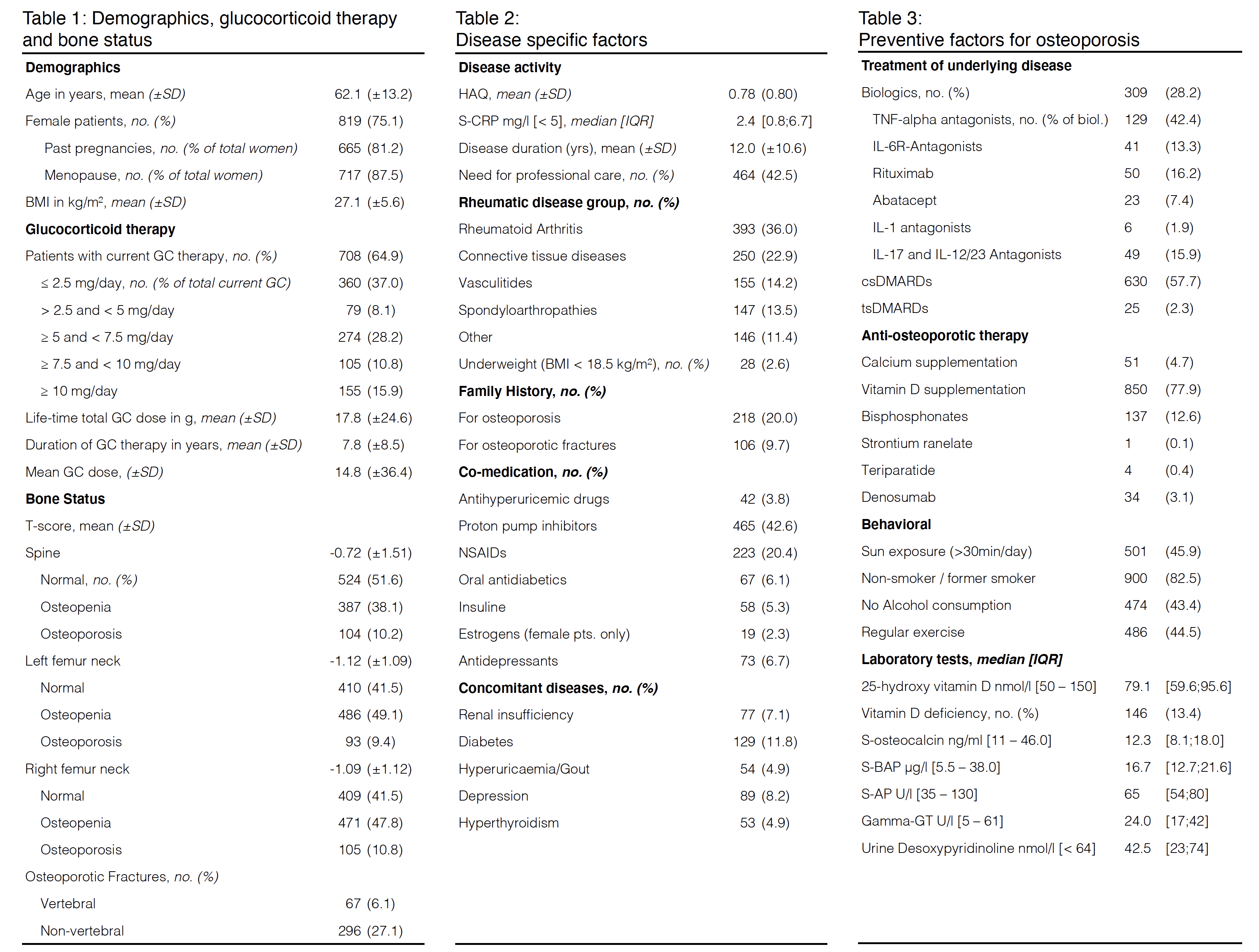
Methods: Rh-GIOP is an ongoing prospective observational study collecting and analyzing disease- and bone-related data from patients with chronic rheumatic diseases or psoriasis treated with GCs. In this cross-sectional analysis, we evaluated the initial visit of 1091 patients.
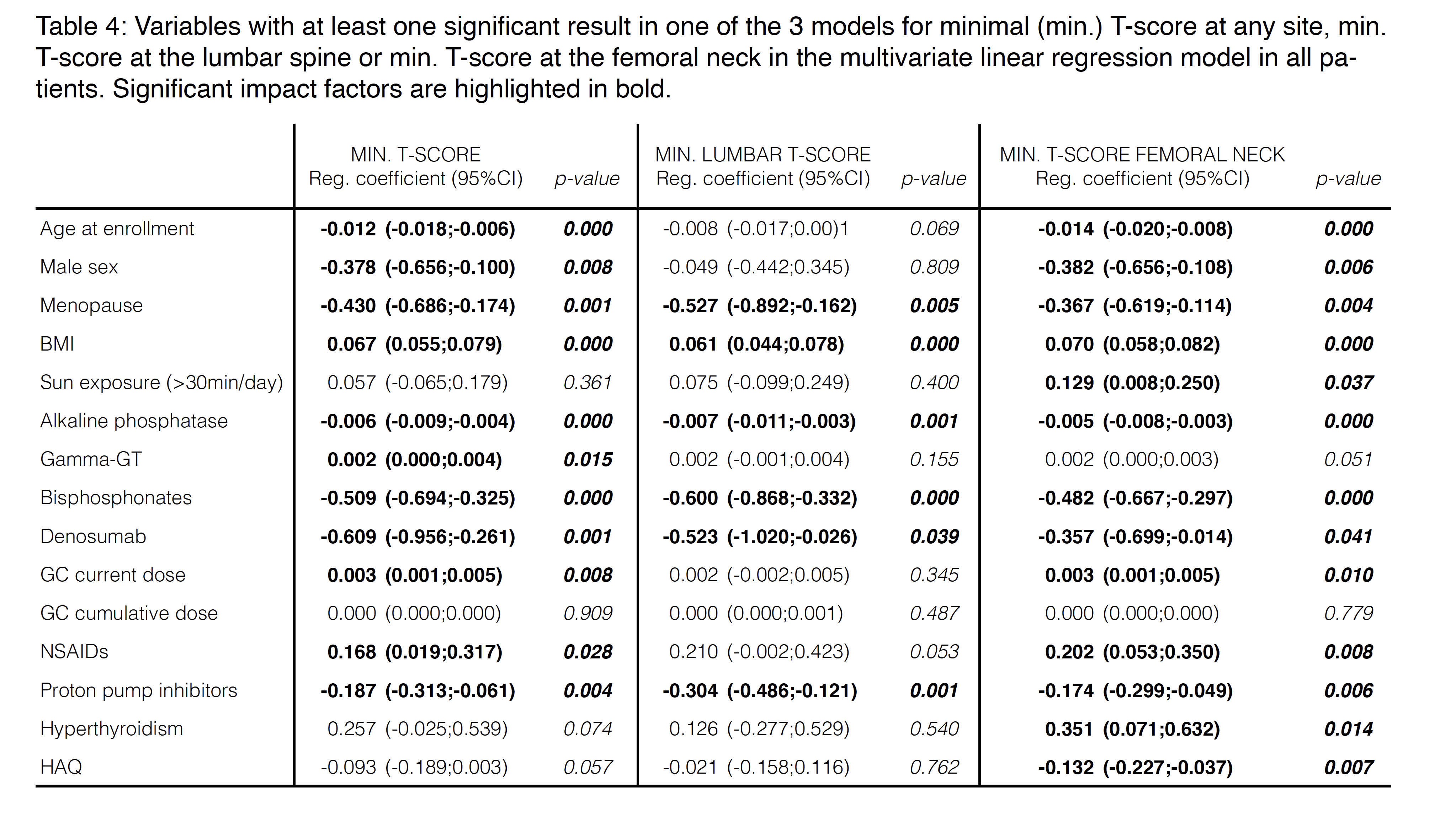
A multivariate linear regression model with known or potentially influential factors adjusted for age and sex was used to identify predictors of BMD as measured by dual-energy X-ray absorptiometry (DXA). Multiple imputation was applied for missing baseline covariate data.
The following T-scores were considered: i) minimum overall T-score, ii) minimum T-score of the lumbar spine and iii) minimum T-score of the femoral neck. P-values lower than 0.05 were considered significant; no adjustment for multiple testing was done.
Results: In the total cohort of 1091 patients (75% female of which 87.5% were postmenopausal) with a mean age of 62.1 (±13.2) years, the prevalence of osteoporosis by DXA was 21.7%, while fragility fractures have occurred in 31.2% of the study population (6.7% vertebral, 27.7% nonvertebral). Current GC therapy was common (64.9%), with a median daily dose of 5.0mg [0.0;7.5], a mean life-time total GC dose of 17.7g (±24.6), and a mean GC therapy duration of 7.8 years (±8.5). Bisphosphonates were the most commonly used anti-osteoporotic drug (12.6%).
BMD as expressed by min T-Score at all measured sites was predicted by age, sex, menopause and BMI, Bisphosphonate and Denosumab treatment, as well as current GC therapy, proton pump inhibitor intake and use of NSAIDs. Current GC dose showed a positive correlation with BMD. Of measured bone-specific laboratory parameters, alkaline phosphatase levels and Gamma-GT were determinants of BMD. BMD was neither predicted by duration of GC treatment, GC cumulative dose nor by treatment with DMARDs or other factors relating to disease activity. Determinants for BMD varied slightly at the anatomical site with HAQ, hyperthyroidism and sun exposure affecting only femoral T-Score.
Conclusion: This cross-sectional analysis of our cohort study revealed a high prevalence of osteoporosis by DXA and fragility fractures. We identified and corroborated predictive variables of BMD that warrant consideration in the management of patients with rheumatic diseases.
To cite this abstract in AMA style:
Wiebe E, Freier D, Huscher D, Hermann S, Biesen R, Buttgereit F. Glucocorticoid-Induced Osteoporosis in Patients with Chronic Inflammatory Rheumatic Diseases: A Multivariate Linear Regression Analysis Identifying Factors Affecting Bone Mineral Density [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/glucocorticoid-induced-osteoporosis-in-patients-with-chronic-inflammatory-rheumatic-diseases-a-multivariate-linear-regression-analysis-identifying-factors-affecting-bone-mineral-density/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/glucocorticoid-induced-osteoporosis-in-patients-with-chronic-inflammatory-rheumatic-diseases-a-multivariate-linear-regression-analysis-identifying-factors-affecting-bone-mineral-density/