Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Osteoporosis is a major cause of morbidity and mortality in the United States. The USPSTF recommends screening all women age 65 and older or younger women with risk factors for osteoporosis.[2] Unfortunately, osteoporosis screening rates remain low nationwide.[3] In our residency clinic, the baseline screening rate for women age 65 and older was 47%. We aimed to increase this rate by 10% over a three month period.
Methods: Our root cause analysis identified provider, patient, and system level barriers to osteoporosis screening. Plan-Do-Study-Act (PSDA) cycle 1 targeted provider knowledge through didactic education and posters in the clinic space. PDSA cycle 2 identified patient barriers. We collaborated with an institutional nurse-led program called “Strong Bones” that has existing initiatives in place to detect and treat osteoporosis. We used a health registry embedded within our electronic medical record to identify patients from our clinic who were eligible for osteoporosis screening. A Strong Bones nurse then reached out to each patient to explain the need for screening and to help navigate barriers. We then tracked the rate of osteoporosis screening between PDSA cycles through the health registry and manually reviewed patient level data during a three month patient outreach period.
Results: After PDSA cycle 1, we saw a slight increase in our screening rate from a baseline of 46% (101/216) to 49% (106/216). During PDSA cycle 2, we identified and chose 138 patients eligible for osteoporosis screening to be contacted. 71 of these patients were called during the outreach period, and 11 scans were completed. Our screening rate at the beginning of cycle 2 was 34% (111/322) and increased to 36% (122/338). The most common barrier identified during this period was patient disinterest, though many were unreachable.
Conclusion: Results from PDSA-1 showed that resident education alone increased the number of DEXA scans ordered, but did not substantially increase completed screenings due to patient barriers. Furthermore, relying on “inreach” interventions targeting only the patients present at the office visit missed a large proportion the patient panel. PDSA cycle 2 addressed both of these issues. There was a substantial increase in DEXA completion and we were also able to quantify the barriers our patients faced in the process. Limitations included difficulty in obtaining reliable data. Additionally, ongoing changes to the health registry’s patient attribution characteristics led to a lower rate of completed screening even though the total number of screenings increased. Although our intervention led to more patients having their screening completed, it was very time-intensive and would be difficult to sustain moving forward. Next steps consist of identifying ways to decrease system level barriers, such as through streamlined scheduling and same day appointments.
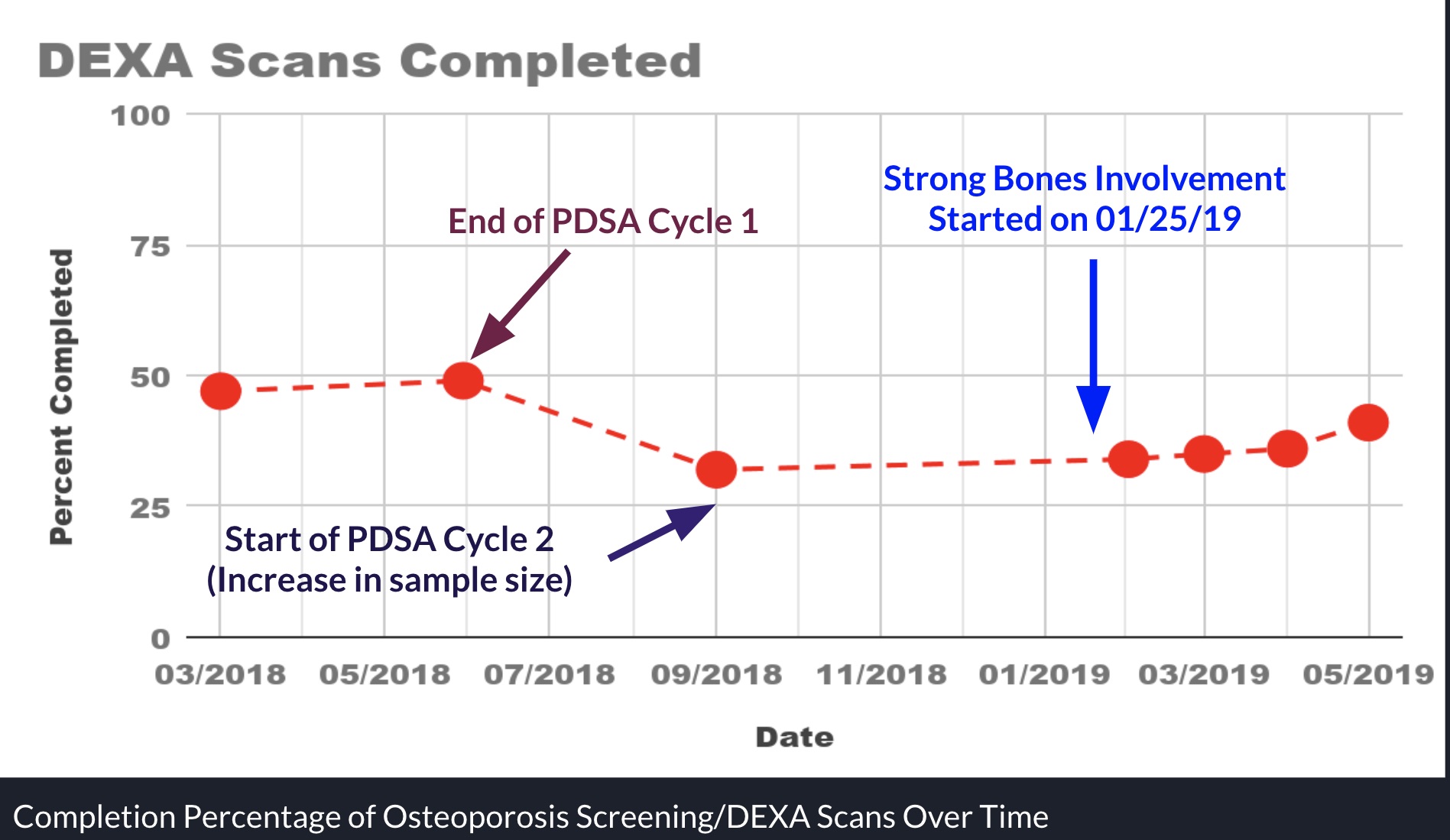 Completion Percentage of Osteoporosis Screening/DEXA Scans Over Time
Completion Percentage of Osteoporosis Screening/DEXA Scans Over Time
To cite this abstract in AMA style:
Teskin C, Sayed H. A Resident-Led Interdisciplinary Quality Improvement Initiative to Increase Osteoporosis Screening in an Urban Clinic [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/a-resident-led-interdisciplinary-quality-improvement-initiative-to-increase-osteoporosis-screening-in-an-urban-clinic/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-resident-led-interdisciplinary-quality-improvement-initiative-to-increase-osteoporosis-screening-in-an-urban-clinic/
