Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Osteoporosis causes significant morbidity, mortality and healthcare burden. There continues to be a care gap in osteoporosis recognition, treatment and prevention. Several healthcare systems in the USA and worldwide have implemented a Fracture Liaison Service (FLS) aimed at secondary fracture prevention. Locally, a 2015-2016 study showed that up to 90% of elderly patients admitted to a tertiary academic center were not screened or treated for osteoporosis. An FLS was established fall 2017 to bridge the care gap in our population. The objective of this study is to longitudinally analyze the effectiveness of the FLS during the initial thirty-month period.
Methods: Data from the electronic health record (EHR) were analyzed to identify the number of inpatient FLS consults received between September 2017and February 2020 (30 months). The following metrics were recorded: demographics, anatomic location of fracture, any prior fractures, calcium and Vitamin D supplementation, pharmacotherapy initiation, DXA completion, transition to osteoporosis specialist and transition to any dependent living facilities. Current data was compared to 8-month data. Main target outcome was a 10% improvement in treatment initiation. Prior data noted that at month 8 and 18 transition to outpatient specialist was delayed, and a significant number of patients (25%) had a primary care provider outside of the academic health system. An FLS nurse practitioner (NP), who also acted as an FLS coordinator, was hired at 18 months. A Chi-square test of independence was utilized to determine if there were proportional differences between those at the 8-month follow-up compared to those at the 30-month follow-up. Alpha was set equal to 0.05 for statistical significance.
Results: 189 patients were referred to the FLS service since initiation (Table 1). A 5% improvement in outpatient follow up was noted at the 30-month mark (32.5%) compared to the 8-month (27.4%) mark (Table 2). Treatment initiation rates that slightly decreased at the 30-month mark were noted to be largely due to patient refusal. This refusal in treatment initiation was noted to be due to patients’ poor understanding of osteoporosis, fracture complications and risk aversion to use of medications. When a comparison was made between the 8-month group with the 30-month group using the chi-square test, no proportional differences in DEXA completed after discharge, transition to outpatient osteoporosis specialist, or osteoporosis treatment initiation after discharge was seen (Table 2).
Conclusion: The number of patients transitioning to outpatient care has improved since the hiring of a NP/FLS Coordinator, even among patients who had a primary care provider outside of the academic health system. However, this number is not statistically significant. A study to analyze patient perceptions about osteoporosis and treatment risk aversion would be useful. Further education efforts are needed aimed at improving osteoporosis awareness not only among patients but also among Primary Care Providers.
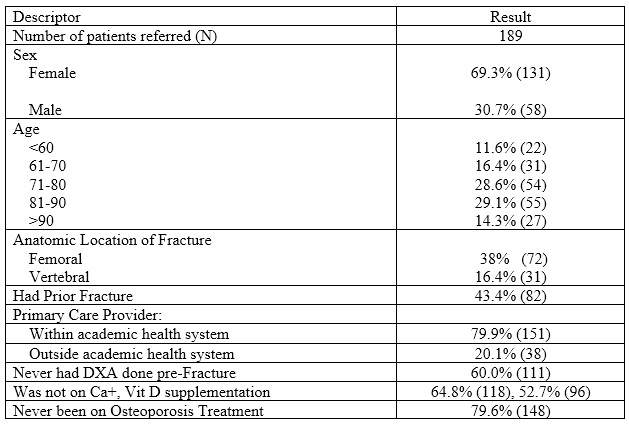 Table 1. FLS Population at an Academic Medical Center associated with an Open Health System at 30 months Data Collection
Table 1. FLS Population at an Academic Medical Center associated with an Open Health System at 30 months Data Collection
 Table 2. Outcome Metrics of a Fracture Liaison Service at an Academic Health System at 8 months and 30 months Data Collection
Table 2. Outcome Metrics of a Fracture Liaison Service at an Academic Health System at 8 months and 30 months Data Collection
To cite this abstract in AMA style:
Jose D, Yu M, Torralba K, Downey C, Dunn J, Cabido V. Fracture Liaison Service at an Academic Center with an Open Health System: 30-month Outcomes [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/fracture-liaison-service-at-an-academic-center-with-an-open-health-system-30-month-outcomes/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/fracture-liaison-service-at-an-academic-center-with-an-open-health-system-30-month-outcomes/
