Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with rheumatoid arthritis (RA) have abnormalities in central nervous system regulation of pain, leading to enhanced pain sensitivity at joint sites (peripheral sensitization) and in a widespread distribution (central sensitization). Pain sensitization is important because it is associated with elevations in composite disease activity measures and patient-reported pain. It is unknown whether treatment with disease modifying anti-rheumatic drug (DMARD) therapy can modify pain sensitization. The objective of this study was 1) to examine changes in pain sensitization in RA following 12 weeks of DMARD therapy and 2) to determine the association between changes in pain sensitization and changes in disease activity.
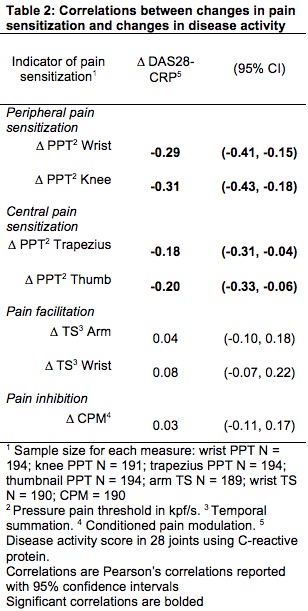
Methods: This study included 236 participants with active RA who were changing DMARD therapy per standard of care. Participants underwent quantitative sensory testing (QST) to assess pressure pain thresholds (PPTs) at the wrist and knee to assess peripheral sensitization and PPTs at the trapezius and thumbnail to assess central sensitization. Temporal summation (TS) was assessed as a specific measure of central sensitization involving pain facilitation, and conditioned pain modulation (CPM) was measured to assess pain inhibition. Disease activity was assessed using the disease activity score in 28 joints using C-reactive protein (DAS28-CRP). Differences in QST measures between baseline and 12-weeks after DMARD initiation were assessed using paired t-tests. Associations between changes in QST measures and changes in DAS28-CRP and its components were assessed with Pearson’s correlation coefficients.
Results: PPTs increased (reflecting lower pain sensitivity) from baseline to follow-up; however, changes were small (ΔPPT wrist = 0.44 kpf/s, p = < 0.0001; ΔPPT knee = 0.43 kpf/s, p = 0.0002; ΔPPT trapezius = 0.37 kpf/s, p = < 0.0001; ΔPPT thumb = 0.44 kpf/s, p=< 0.0001) (Table 1). TS and CPM did not change significantly from baseline to follow-up. Negative correlations between changes in PPTs and changes in DAS28-CRP were strongest at joint sites (wrist r = -0.29, 95% confidence interval (CI) = -0.41 to -0.15; knee r = -0.31, 95% CI = -0.43 to -0.18) and weaker at non-joint sites (trapezius r = -0.18, 95% CI = -0.31 to -0.04; thumb r = -0.20, 95% CI = -0.33 to -0.06) (Table 2). Changes in TS or CPM were not significantly correlated with changes in DAS28-CRP.
Conclusion: All PPTs increased with DMARD treatment reflecting decreasing pain sensitivity. Correlations with DAS28-CRP were strongest with measures of peripheral sensitization. This is consistent with the idea that peripheral sensitization is driven by joint inflammation. However, changes in PPTs were small in magnitude. Treatment with DMARDs alone may not be sufficient to address pain sensitization in RA.
To cite this abstract in AMA style:
Heisler A, Song J, Muhammad L, Wohlfahrt A, Marder W, Bolster M, Bingham III C, Clauw D, Dunlop D, Neogi T, Lee Y. Association Between Changes in Pain Sensitization and Changes in Disease Activity After 12 Weeks of Disease Modifying Anti-Rheumatic Drug Therapy in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/association-between-changes-in-pain-sensitization-and-changes-in-disease-activity-after-12-weeks-of-disease-modifying-anti-rheumatic-drug-therapy-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-changes-in-pain-sensitization-and-changes-in-disease-activity-after-12-weeks-of-disease-modifying-anti-rheumatic-drug-therapy-in-rheumatoid-arthritis/