Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Frailty, a state of decreased homeostatic reserve, is associated with increased disability and mortality, independent of age. Frailty has been evaluated in large datasets using validated algorithms in the elderly. Although frailty has been investigated in several rheumatic diseases, including RA, to our knowledge, frailty has not been investigated in AS and PsA, which often affect younger patients. In this study, we evaluated the prevalence of frailty among patients < 65 years old with AS and PsA compared to RA in a national claims database.
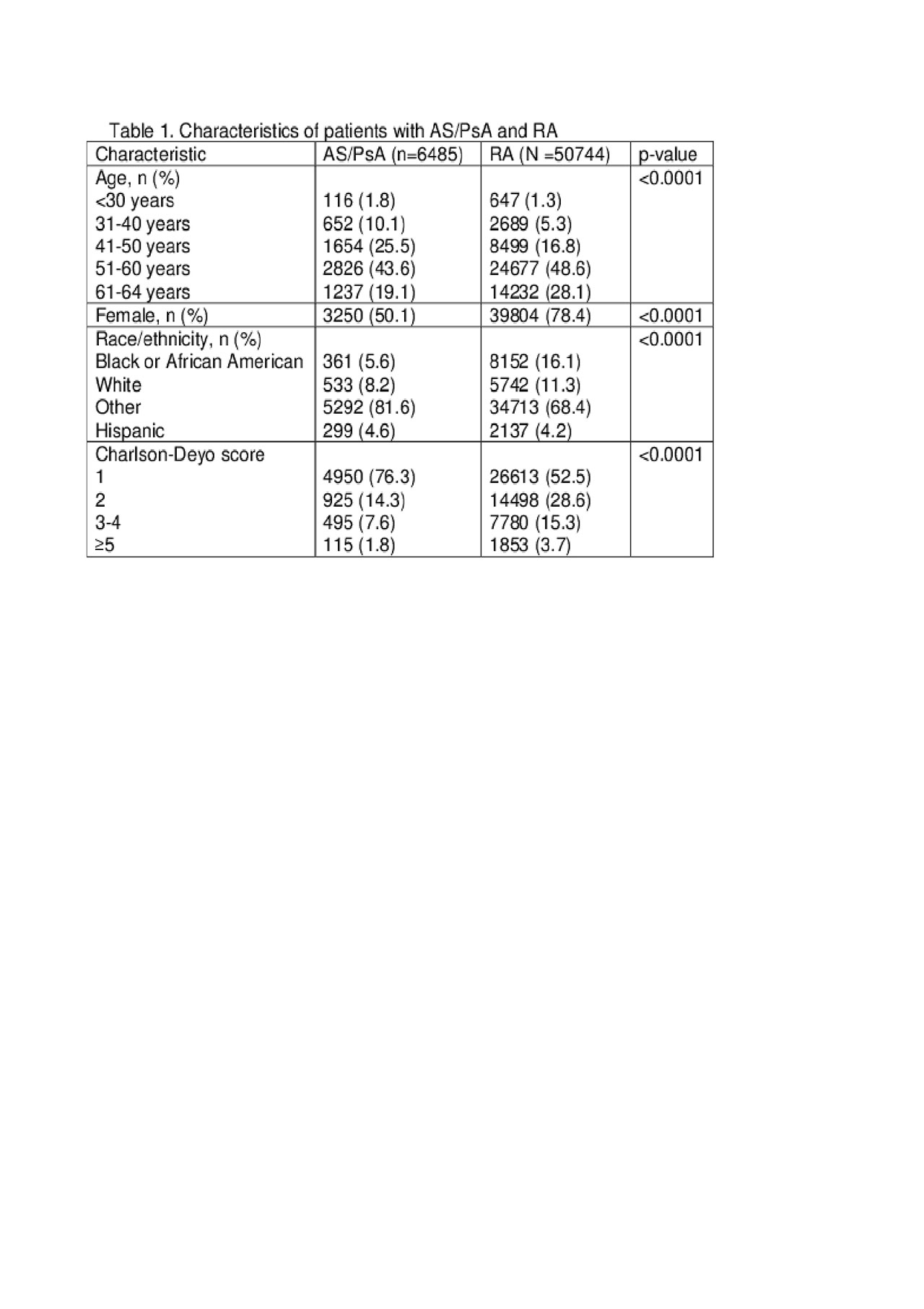
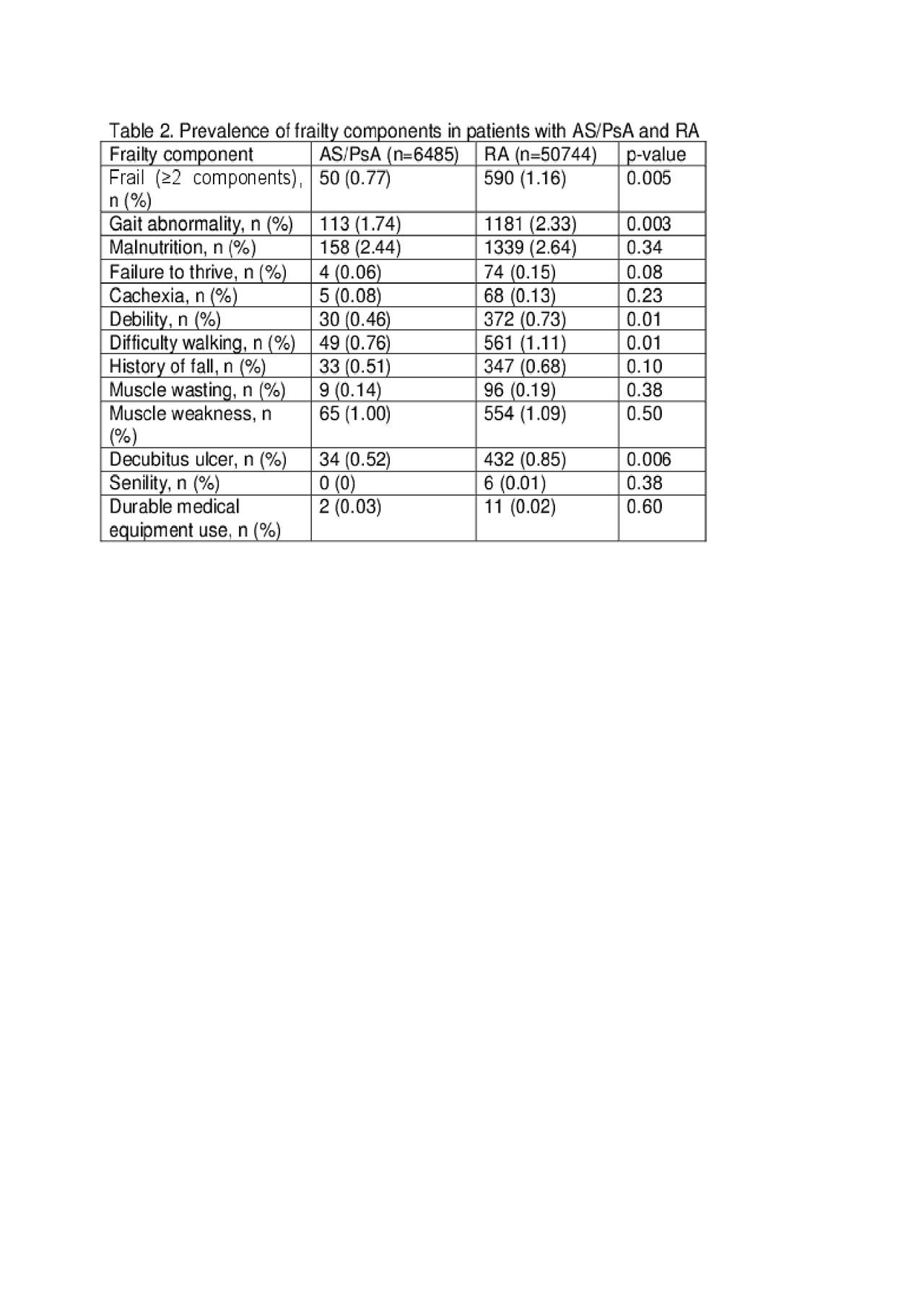
Methods: We performed a cross sectional study of Centers for Medicare and Medicaid Services (CMS) Medicare beneficiaries (Part A and B) from 2014 who were < 65 years old. Patients with an ICD-9-CM code for AS, PsA, or RA on 2 occasions ≥7 days apart within a year or 1 ICD-9-CM code and ≥1 DMARD prescription (from Part D) were included. Patients with SLE, IBD, cancer, human immunodeficiency virus, end stage renal disease, skin psoriasis, or organ transplantation were excluded. Sociodemographic characteristics, Charlson-Deyo score (CDS), and previously published frailty components [1] were compared between those with AS/PsA and RA. Frailty was defined as presence of ≥2 components [1] (Table 2). Logistic regression was used to determine the odds of being frail in AS/PsA and RA, adjusting for age, gender, race/ethnicity, and CDS.
Results: 6485 AS/PsA and 50744 RA beneficiaries were identified. AS/PsA patients were more often white (81.6% v. 68.4%, p< .0001), male (49.9% v. 21.6%, p< .0001), and younger (37.4% v. 23.3% ≤ 50 years old, p< .0001) as compared to those with RA (Table 1). Enrollees with AS/PsA had lower CDS than those with RA (p< .0001). Fewer patients with AS/PsA were frail (0.77%) compared to those with RA (1.16%) (p=.005) (Table 2). Several frailty components, including gait abnormality (p=.003), debility (p=.01), difficulty walking (p=.01), and decubitus ulcer (p=.006), were less common in those with AS/PsA. After adjustment for confounders, odds of frailty did not differ significantly between AS/PsA (OR 0.89, 95% CI 0.66-1.20) and RA.
Conclusion: The prevalence of frailty in AS/PsA was lower than that in RA; however, odds of frailty were similar in both groups after adjustment for confounders. The prevalence of frailty in RA was lower than in prior cohorts of young RA patients [2-3], possibly suggesting that this frailty definition may underestimate frailty prevalence. Data analysis is ongoing to compare these findings with models using other validated frailty algorithms. It will be important to have accurate frailty estimates to leverage the information in large administrative datasets to optimize patient outcomes.
1. Joynt et al. 2017
2. Haider at al. 2018
3. Cleutjens et al. 2018
To cite this abstract in AMA style:
Lieber S, Rajan M, Sattui S, Lui G, Schwartzman S, Mandl L, Navarro-Millan I. Frailty in Ankylosing Spondylitis, Psoriatic Arthritis, and Rheumatoid Arthritis: Data from a National Claims Database [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/frailty-in-ankylosing-spondylitis-psoriatic-arthritis-and-rheumatoid-arthritis-data-from-a-national-claims-database/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frailty-in-ankylosing-spondylitis-psoriatic-arthritis-and-rheumatoid-arthritis-data-from-a-national-claims-database/