Session Information
Date: Tuesday, November 12, 2019
Title: Patient Outcomes, Preferences, & Attitudes Poster II: Patient Preferences, Beliefs, & Experiences
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Evidence-based guidelines recommend escalation of therapy in patients with rheumatoid arthritis (RA) with inadequately controlled disease. However, some patients are hesitant to change therapies despite significant symptom burden. Understanding the patient factors that are associated with willingness to change therapy may inform the design of behavioral interventions to improve appropriate escalation of treatment in patients with RA.
Methods: Adult patients with self-reported RA who were enrolled in the ArthritisPower patient registry with a RAPID3 > 4 (range 0-10), treated with DMARDs in the past 6 months, and without potentially confounding conditions (e.g. fibromyalgia) were eligible to participate in the Confident Treatment Decisions for Living with Rheumatoid Arthritis (CONTROL RA) clinical trial. Patients were recruited by email to complete a compensated online survey. Participants’ willingness to change RA treatment was determined at enrollment using the validated choice predisposition scale that reflects preference for changing RA therapies. Patients were asked “If at your next visit, your rheumatologist recommends that you change RA medication(s), would you be willing to do so?” This item was coded on an 11-point scale anchored by “Not willing at all” and “Extremely willing”. Patients who answered 7-10 were categorized in the “more willing to change treatment” group, while those with a score of 0 – 6 were classified in the “less willing to change treatment” group. Bivariate tests and multivariable logistic regression evaluated the following characteristics associated with these two levels of willingness to change treatment: sociodemographic characteristics, biologic DMARD or conventional DMARD use, patient global assessment of disease activity (PGA), patient satisfaction with RA control, (yes vs no) personal attitudes favoring RA medications (calculated by surveying participants’ agreement with 5 positive and 5 negative statements about use of medications in RA. Higher score represents more favorable attitude towards RA medications), patient-physician discussion on RA treatment goals occurring in the past year, subjective characterization of general health (5 point scale anchored by “excellent” and “poor”), and subjective readiness to change (Precaution Adoption Process Model). Subjective health literacy calculated by asking patients about their confidence in filling out medical forms.
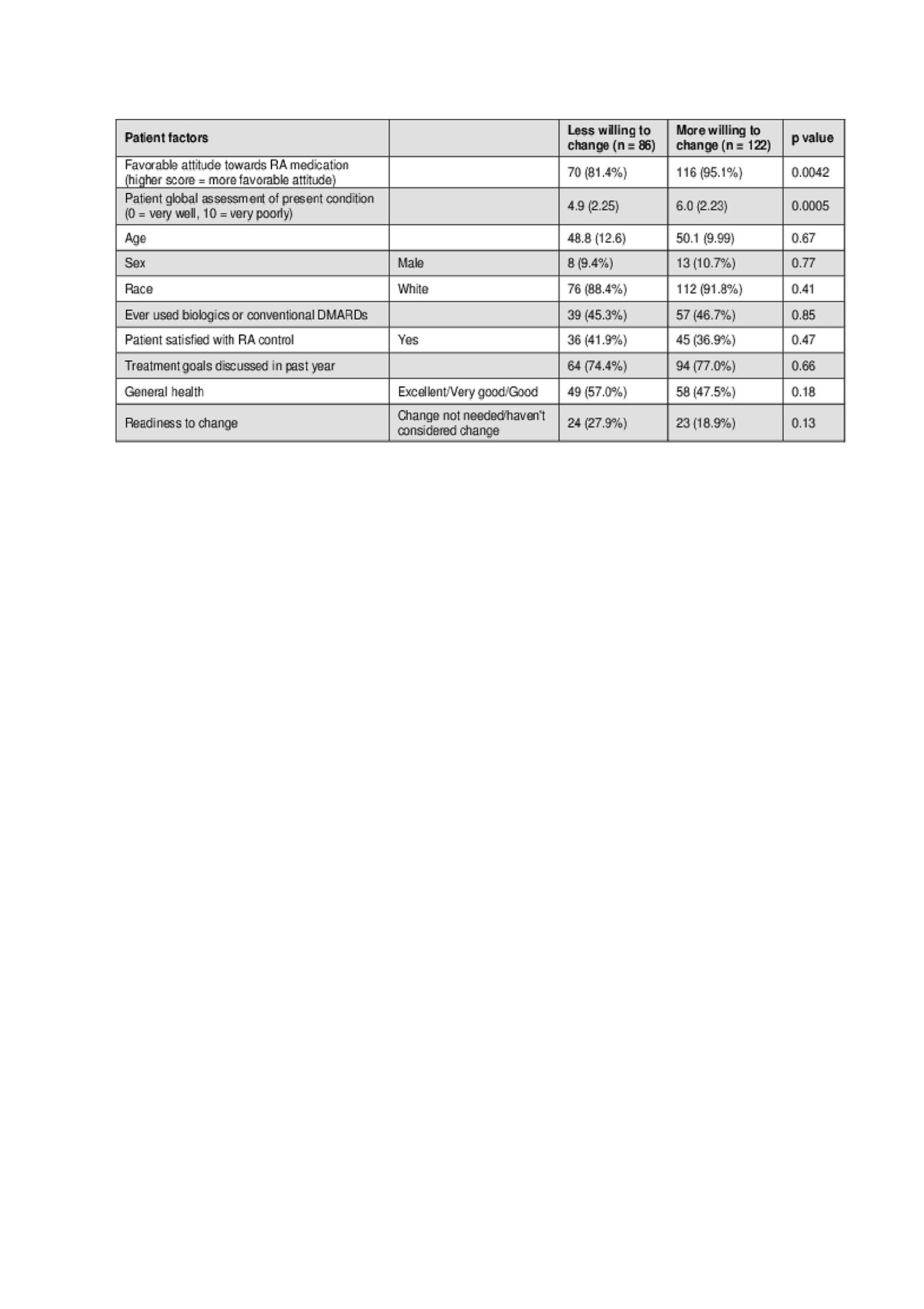
Results: A total of 208 U.S. patients were recruited. Study participants were 90% Caucasian, 90% women, with high subjective health literacy and a mean (SD) age of 50 (11) years. In adjusted models, we found that compared to the less willing group, participants in the more willing to change group were more likely to have a higher PGA (OR 1.4 p = 0.0006, CI 1.1 – 1.6), and more likely to have a favorable attitude towards RA medication than those in the less willing group (95.1% vs 81.4%, p = 0.0042; OR 7.0, p = 0.0008, CI 2.2 – 21.8).
Conclusion: Our study suggests that among patients with self –reported RA, having attitudes that favored RA medications and a higher patient global assessment of disease activity were independently associated with an increased willingness to change RA medications.
To cite this abstract in AMA style:
Vachhani R, Chen L, O'Beirne R, Melnick J, Ruderman E, Curtis J, Danila M. Patient Factors Associated with Willingness to Change Rheumatoid Arthritis Medications [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/patient-factors-associated-with-willingness-to-change-rheumatoid-arthritis-medications/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-factors-associated-with-willingness-to-change-rheumatoid-arthritis-medications/