Session Information
Date: Tuesday, November 12, 2019
Title: Epidemiology & Public Health Poster III: OA, Gout, & Other Diseases
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The burden of co-morbid conditions can impact the overall quality of life in patients with RA and OA. However, the presence of common co-morbidities in inflammatory and degenerative arthritis is not well described. We sought to compare overlapping co-morbidities in the two patient groups.
Methods: We identified patients with physician-diagnosed OA and RA in FORWARD, The National Databank for Rheumatic Diseases, a large US registry with comprehensive 6-month questionnaires from 1998 through 2018, with patients primarily recruited through rheumatology clinics. Each patient with OA was age- and sex-matched to two patients with RA at study entry. We compared demographics, clinical characteristics and current and past co-morbidities between the OA and RA groups. Patient status at the last observation was further categorized as active (if they had a full follow-up questionnaire collected in the last 2 years), not active, or lost to follow-up/deceased. T-tests and Chi-square tests were used as appropriate to assess differences.
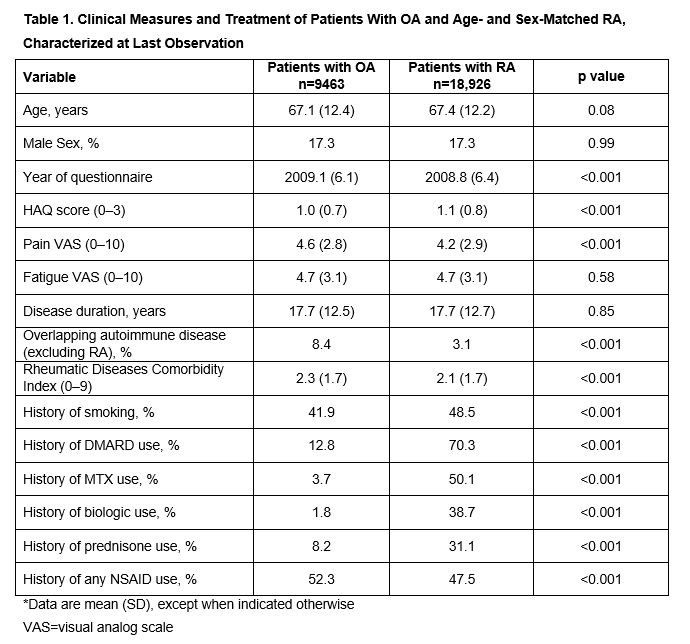
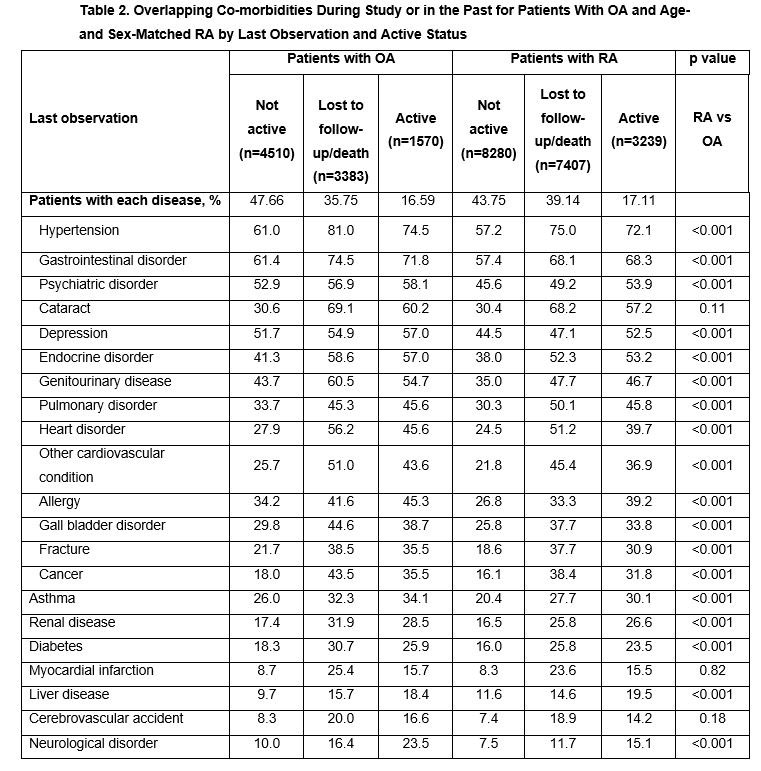
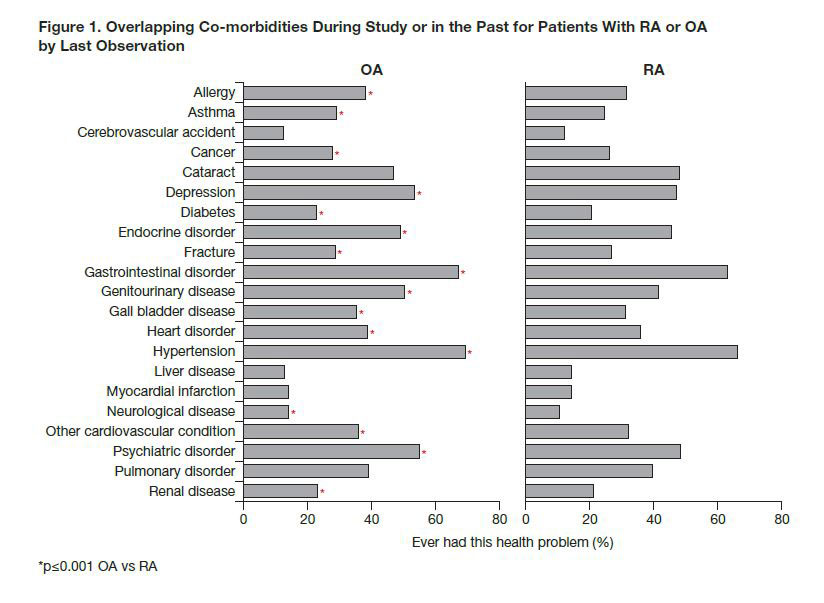
Results: Overall, 9463 patients with OA were matched to 18,926 patients with RA. Patients with OA experienced more pain compared with patients with RA (4.6 vs 4.2), but patients with RA had slightly worse HAQ scores (1.0 vs 1.1; Table 1). Higher use of NSAIDs was reported for patients with OA. Except for pulmonary and liver disorders, which were more prevalent among patients with RA, patients with OA had a higher prevalence of the majority of co-morbidities, with an average overall disease co-morbidity index of 2.3 vs 2.1 for patients with RA. Presence of overlapping autoimmune disease was also higher for patients with OA (OA vs RA: 8.4% vs 3.1%). The most frequently reported co-morbidities (OA vs RA) were hypertension (69% vs 66%), gastrointestinal disorders (67% vs 63%) and psychiatric disorders (55% vs 48%) (Figure 1). As expected, patients who were lost to follow-up/deceased had worse outcomes and more co-morbidities than active and non-active patients both with OA and RA. Patients who were not active had more co-morbidities than active patients, revealing an informative drop-out (Table 2).
Conclusion: Patients with OA reported more overlapping co-morbidities than patients with RA, even after age- and sex-matching. Although RA has a much more complex etiology, affecting more organ systems, our data suggest that the burden of having OA in terms of overlapping symptoms and other problems is not negligible in comparison. It is possible that the advancement of medications for RA has aided in lessening the burden of disease or other co-morbidities when compared with OA. Also, this OA cohort may have increased disease severity due to seeking care from a rheumatologist.
Professional medical writing: Katerina Kumpan, Caudex, funded by Bristol-Myers Squibb.
To cite this abstract in AMA style:
Pedro S, Schumacher R, Dominique A, Shaw Y, Wipfler K, Michaud K. Co-morbidities in Patients with OA and RA: Results from a Large US Rheumatic Disease Registry [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/co-morbidities-in-patients-with-oa-and-ra-results-from-a-large-us-rheumatic-disease-registry/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/co-morbidities-in-patients-with-oa-and-ra-results-from-a-large-us-rheumatic-disease-registry/