Session Information
Date: Monday, November 11, 2019
Title: 4M125: Pediatric Rheumatology: Outcomes & Quality of Life (1920–1925)
Session Type: ACR/ARP Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: There is a paucity of literature on the challenges children with JIA face at school. Despite treatment advances, children with JIA often rate their Quality of Life (QoL) and school experience as lower than healthy peers. Absences due to disease flares, office visits, medication administration, or side effects may impact school experience. Training of school nurses on other chronic diseases has led to increased knowledge and management skills as well as improvement in children’s QoL and school experience. Due to the lack of data on school nurses’ awareness about the care of children with JIA, we aimed to improve their knowledge.
Methods: A pediatric rheumatologist presented to school nurses from two large, urban school districts attending a yearly educational seminar. The talk focused on JIA symptoms, course, and treatment, described challenges children with JIA face at school, and recommended accommodations/resources for families and school personnel. Pretest and posttest surveys were administered. Surveys assessed nurses’ knowledge of JIA, any prior experience caring for children with JIA or other chronic conditions, assessed acquired knowledge, and responses to hypothetical cases. The study was approved by the primary institution’s IRB and the local school districts.
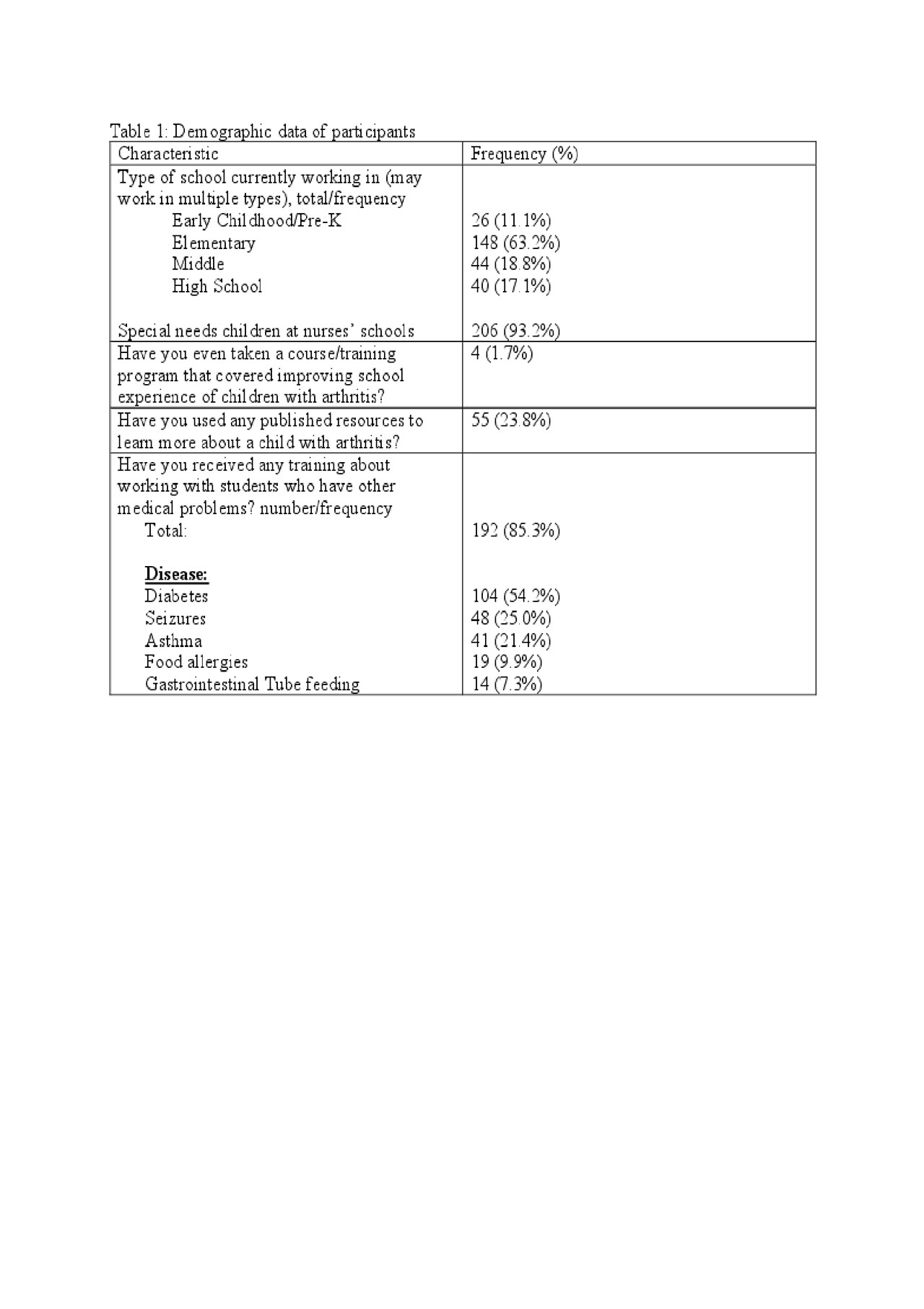
Results: Two hundred and ninety-four school nurses attended the talks. Two hundred and sixty-one nurses (83%) completed both pre and posttest surveys. Most nurses were experienced (mean experience in school setting, 8.8 years, + 8.7) and were predominantly located at elementary schools. They had variable exposure to other pediatric disorders (Table 1). Only 18.3% of nurses had ever met with a caregiver of a child with JIA, and only 11.8% had implemented a JIA health plan. Over 80% of nurses reported no experience in treating JIA, but reported experience treating Diabetes Mellitus (DM). Nevertheless, nurses identified other resources for managing children with JIA in school, such as supportive care and contacting parents. Seventy percent of respondents reported feeling more prepared to treat DM (vs JIA). After the presentation, nurses felt significantly more prepared to care for a child with JIA at a level that was comparable to DM knowledge (Table 2). Nurses’ reported takeaways from the talk included “being more prepared,” “more observant,” and not “dismissing joint complaints in a child with JIA.” The majority (86.3%) of school nurses found the educational session to be useful.
Conclusion: This study highlights school nurses’ knowledge gap regarding JIA in school-age children. We demonstrated the effectiveness of a single educational session to increase knowledge of JIA and influence future care of children with JIA in school. Additional data is necessary to assess nurses’ knowledge retention and practice changes over time. Similar educational interventions for teachers, social workers, or administrators could be used for other autoimmune and autoinflammatory disorders. Efforts to improve the QoL of patients with JIA should involve interdisciplinary “front-line” team members (e.g., medical, mental health, and school personnel). This project can be continued by future trainees to provide community education.
To cite this abstract in AMA style:
Lapin W, Kutac C, Guttman-Lapin D, Brown A, Muscal E, Seeborg F. School Nurse Education for Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/school-nurse-education-for-juvenile-idiopathic-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/school-nurse-education-for-juvenile-idiopathic-arthritis/