Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Many RA patients in clinical remission have evidence of bone marrow edema (BME) on magnetic resonance imaging (MRI), with radiographic bone damage progression appearing in a subset of patients.1 While MRI provides excellent visualization of subclinical inflammation, bone resolution is relatively poor, limiting the correlation of inflammatory imaging findings to erosive change that may develop. High resolution peripheral quantitative computed tomography (HR-pQCT) provides superior detailed bone resolution, with improved erosion detection and quantification. The purpose of this study was to determine whether subclinical inflammation observed on MRI could be co-localized with erosive change visualized by HR-pQCT, thereby predicting bone damage progression over a 6-month follow-up period for RA participants in clinical remission.
Methods: Nine participants meeting the ACR/EULAR criteria for RA and in clinical remission were recruited to undergo contrast-enhanced MRI and HR-pQCT scans of the hand at two timepoints, six months apart. Disease activity between these timepoints was assessed monthly by questionnaire, examination, and inflammatory biomarkers. A multimodal image registration technique was developed to co-localize imaging findings on HR-pQCT and MRI. Synovitis and BME were assessed semi-quantitatively with MRI using the RAMRIS scoring system.2 Bone erosion volume quantification was completed using a 3D segmentation technique using MIAF-Finger3, with joint space width (JSW) assessed using a volumetric approach from HR-pQCT images.4 Individual changes in HR-pQCT outcomes were compared against the least significant change (LSC) measured from scan-rescan reproducibility.
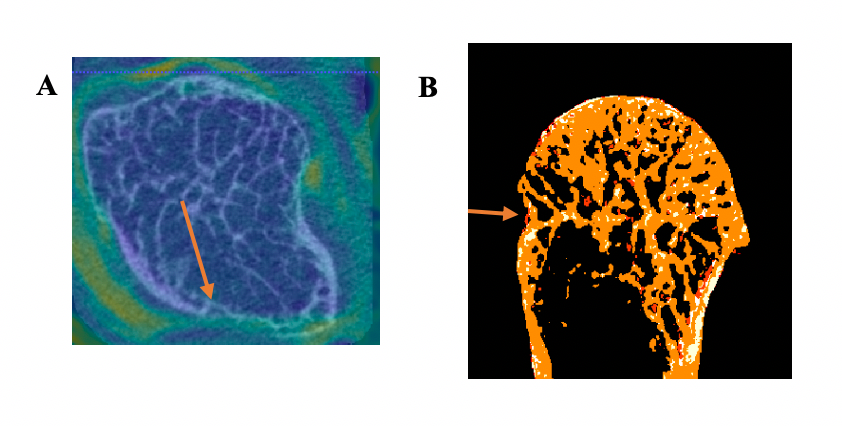
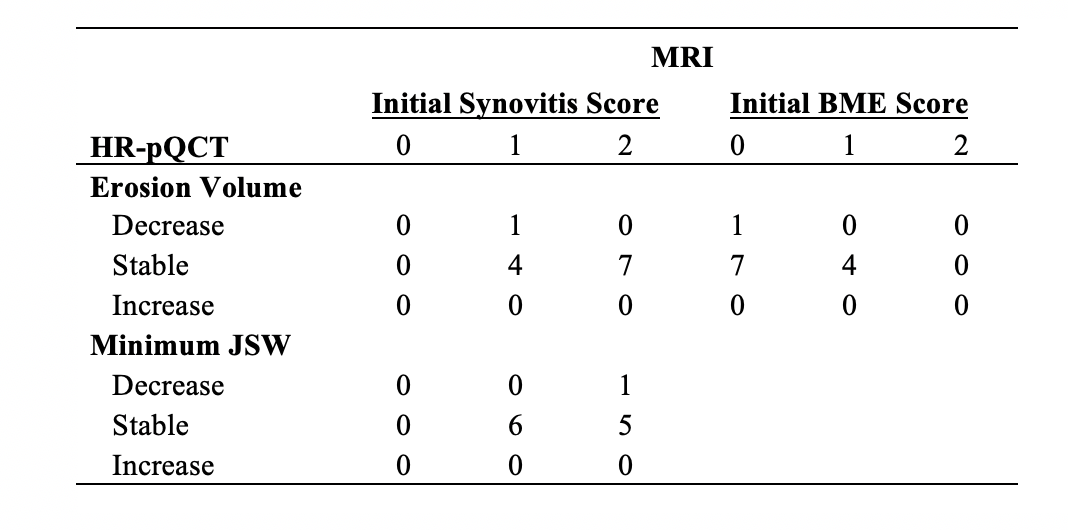
Results: The mean DAS28 for the 9 participants was 2.16 (SD 0.64) at the initial scan and 1.72 (SD 0.76) at follow-up. All participants had evidence of synovitis on MRI. Eight joints had evidence of BME at baseline. Twelve 2nd and 3rd MCP joints seen on HR-pQCT were co-localized with MRI using image registration (Figure 1). The presence of BME did not predict significant change in erosion volume (Table 1). In contrast, absence of BME and synovitis at the location of the erosion was associated with a decrease in erosion volume in one participant (Figure 2). The JSW outcomes remained stable in all joints, with the exception of one joint that showed a decrease in minimum JSW and another that had a decrease in the maximum JSW.
Conclusion: Even with highly sensitive imaging we did not detect erosive progression over the course of 6 months in patients with subclinical inflammation. However, the absence of localized subclinical inflammation was suggested to predict erosion healing. Findings will be confirmed in a larger cohort. This novel image registration technique for RA was able to co-localize areas of subclinical inflammation on MRI with joint damage on HR-pQCT, which could provide insights on the mechanisms of damage in RA that is not possible with either imaging approach alone.
References: 1. Brown, A. K. et al. Arthritis Rheum. 2008. 2. Østergaard, M. et al. Ann. Rheum. Dis. 2005. 3. Töpfer, D. et al. Rheumatol. (United Kingdom). 2014. 4. Stok, K. S. et al. J. Rheumatol.2017.
To cite this abstract in AMA style:
Brunet S, Salat P, Hazlewood G, Engelke K, Barnabe C, Manske S. The Relationship Between Subclinical Inflammation and Bone Damage in Patients with Rheumatoid Arthritis Using Multimodality Imaging [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-relationship-between-subclinical-inflammation-and-bone-damage-in-patients-with-rheumatoid-arthritis-using-multimodality-imaging/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-relationship-between-subclinical-inflammation-and-bone-damage-in-patients-with-rheumatoid-arthritis-using-multimodality-imaging/