Session Information
Date: Sunday, November 10, 2019
Title: Pediatric Rheumatology – ePoster I: Basic Science, Biomarkers, & Sclerodermic Fever
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Down syndrome associated Arthritis (DA) is 20 times more common than JIA. It is an erosive, polyarticular RF negative arthritis with predominance in the small joints of the hands and wrists. Little is known about the underlying mechanisms that drive DA pathogenesis. We hypothesise that it is a distinct disease from its closest ILAR subtype, polyarticular RF negative JIA (pRF-JIA) given the differences observed in the clinical phenotypes.
Our aims were to compare B cell subsets and T cell cytokine profiles in peripheral blood mononuclear cells (PBMCs); and synovial membrane immunohistochemistry and synovial fibroblast cell (SFC) functionality in children with DA and the ILAR subtype pRF-JIA. We also looked to see if known pRF-JIA susceptibility loci, HLA-DQB1/HLA-DQA2 (rs7775055) and PTPN22 (rs6679677) were present in children with DA.
Methods: Multicolour flow cytometry and FlowJo and SPICE software were used to analyse B cell subsets and T cell cytokine expression (IL17a, GMCSF, IFNγ, TNFα) in PBMCs from children with pRF-JIA, DA, T21 and HC, (n = 10 / gp).
Synovial tissue was obtained through ultrasound guided biopsy (DA n = 3; pRF-JIA n = 4) and analysed by immunohistochemistry for CD3 (T cells), CD20 (B cells) and CD68 (macrophages). Vascularity and lining layer hyperplasia were also scored.
DA-SFC and pRF-JIA-SFC migration was assessed by wound repair scratch assays; invasion by Biocoat Matrigel™ Invasion Chambers; and bioenergetic activity using the XFe96-Flux-analyser where oxidative phosphorylation and glycolysis were quantified. Real-time PCR assessed glycolytic gene expression.
The team at the Arthritis Research UK Centre for Genetics and Genomics (Manchester) performed genotyping and analysis of rs7775055 and rs6679677 in DNA from children with pRF-JIA (n = 732), DA (n = 42), T21 (n = 31) and HC (n = 9196).
Results: Flow cytometry analysis revealed that children with DA had a significantly lower number of circulating CD19+CD20+ B cells when compared to children with pRF-JIA and HC. However, they had a greater proportion of memory B cells (CD27+) when compared to children with T21. T cell IFNγ and TNFα production was significantly greater in DA compared to pRF-JIA and HC. Greater T cell polyfunctionality was also observed in children with DA compared to all three comparison groups.
DA synovial tissue demonstrated greater lining layer hyperplasia (figure 1). Median cell thickness in DA was 6 (3-9 cells), compared to 2 (2-4 cells) in pRF-JIA. There was also increased vascularity and inflammatory cell infiltration in DA compared to pRF-JIA.
DA-SFC showed greater migratory and invasive capacity, and increased basal metabolic activity and metabolic gene expression when compared to pRF-JIA-SFC.
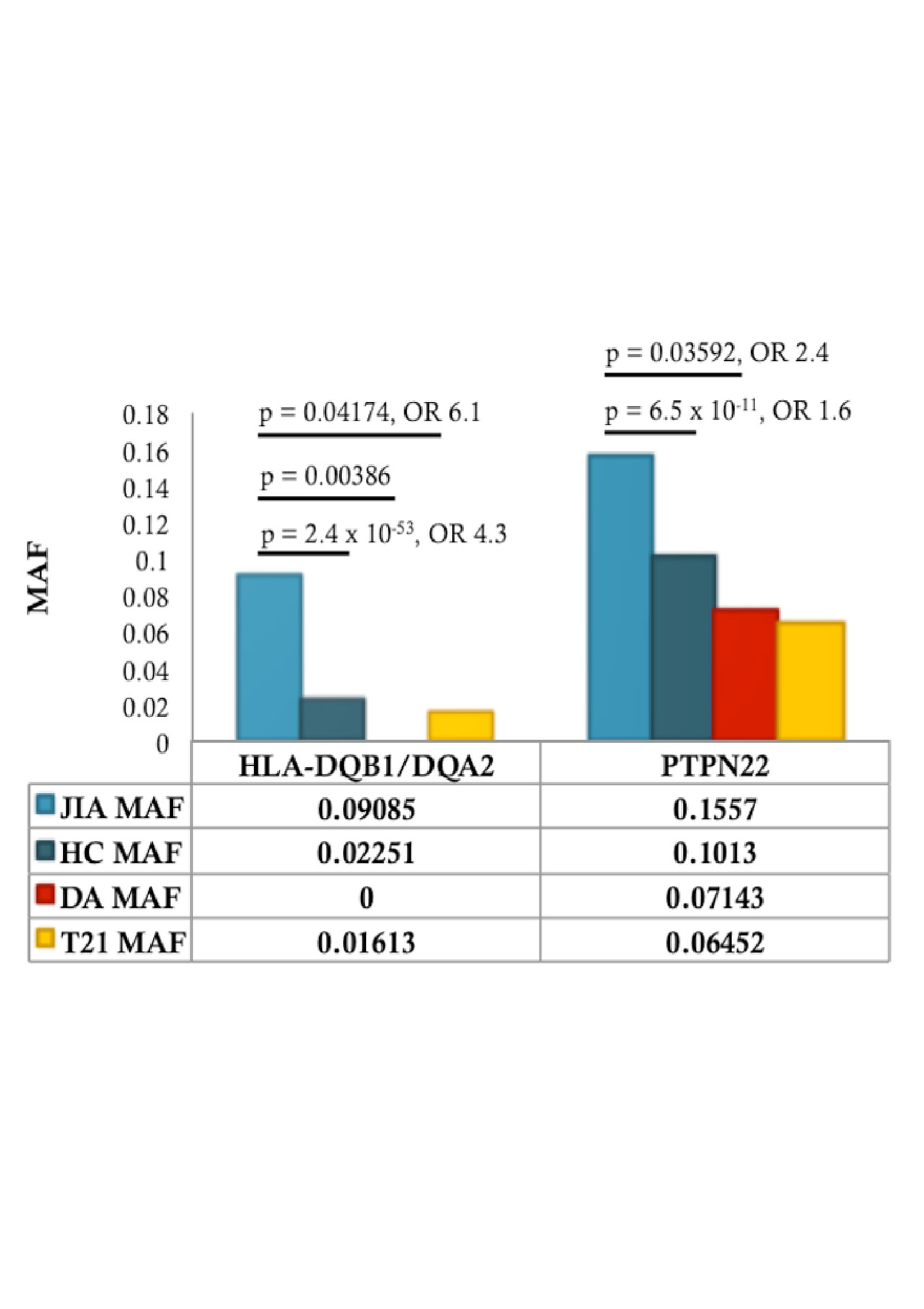
The MAF (minor allele frequency) for the pRF-JIA associated variants rs7775055 and rs6679677 were not similar in DA. The minor allele of rs7775055 was absent in DA (p = 0.004). The rs6679677 MAF was significantly different between DA and pRF-JIA, p = 0.036 (figure 2).
Conclusion: Significant differences were observed in the immune, histological and genetic profiles of DA and its closest ILAR subtype, pRF-JIA. These differences may help explain the erosive phenotype observed in DA and suggest it may be a distinct disease from JIA.
A. Representative images of synovial tissue from the knee joint of a child with DA and JIA. The black line denotes lining layer. B. Two independent observers performed scoring. Graphs depict results for global inflammation and vascularity, with a score range of 0-3. Lining layer thickness was scored by number of cells thick. Sample size was DA n = 3 and JIA n = 4. Original magnification used was 20 X. Data are presented as mean ± SEM.
Comparable to the literature, the MAF for HLA-DQB1/HLA-DQA2 -rs7775055- in JIA is significantly greater than HC -p=2.4 x 10-53, OR 4.3-. When compared to HC, both T21 and DA have a lower MAF. Results for these cohorts are significantly lower when compared to JIA MAF -p=0.04174 and p=0.00386 respectively-. Similarly, for PTPN22 -rs6679677-, MAF in JIA is significantly greater than HC -p=6.5 x 10-11, OR 1.6-. Again, in both the T21 and DA cohort, MAF is lower compared to HC. DA MAF is significantly lower than JIA MAF -p=0.03592, OR 2.4- for this JIA susceptibility locus.
To cite this abstract in AMA style:
Foley C, Floudas A, Ansboro S, Canavan M, Biniecka M, MacDermott E, Mullan R, Wilson G, Fearon U, Killeen O. Is down Syndrome Associated Arthritis (DA) a Distinct Disease from Juvenile Idiopathic Arthritis (JIA)? [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/is-down-syndrome-associated-arthritis-da-a-distinct-disease-from-juvenile-idiopathic-arthritis-jia/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-down-syndrome-associated-arthritis-da-a-distinct-disease-from-juvenile-idiopathic-arthritis-jia/