Session Information
Date: Sunday, November 10, 2019
Title: Education Poster
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The maneuvers to include in a comprehensive shoulder exam are debatable. For rheumatology fellows, rheumatology fellowship program directors (PD) serve as models of competency in performing the musculoskeletal exam. In this pilot study, we investigated exam techniques used by PDs in comparison to rheumatology fellows in their first year of training.
Methods: We recruited 6 rheumatology clinic patients with known causes of shoulder pain to undergo physical exam by 3 rheumatology PDs (32-36 years post medical school), and 3 rheumatology fellows in the first 3 months of training (3-4 years post medical school). Exams were performed in a simulation center with video recording. Exam procedure was not standardized beforehand, but fellows had formal training in shoulder exam both before and during fellowship. Overall diagnosis was noted by participants after each exam. Ultrasound imaging on the day of the exercise and clinical information were used to establish a “gold standard” (GS) diagnosis for each patient.
Videos were reviewed by a 4th PD using a standardized data extraction tool (27 exam techniques) based on a previously published standardized observed clinical exam (OSCE) of the shoulder. Exam findings not included in this tool, as well as total exam duration per room were also recorded.
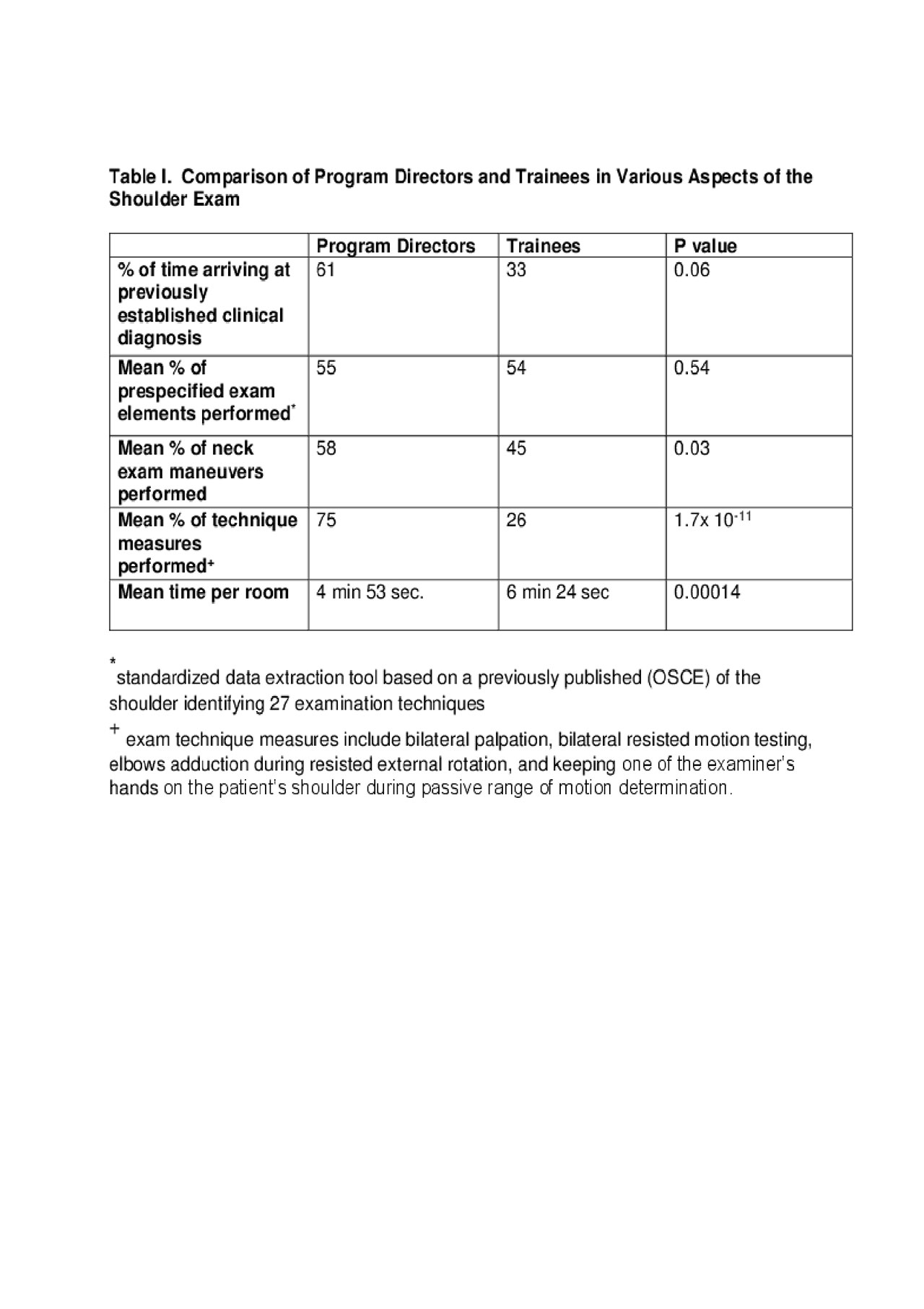
Exam maneuvers employed for each patient, technical methodology of the maneuvers, agreement with GS diagnosis, and duration of each exam were compared between the two groups using the student-t test. Four measures of exam technique assessed for each encounter included bilateral palpation, bilateral resisted motion testing, elbows adducted during resisted external rotation, and keeping one of the examiner’s hands on the patient’s shoulder during passive range of motion testing.
Results: GS diagnoses were: biceps tendonitis (x2), acromioclavicular joint arthritis, adhesive capsulitis, subacromial bursitis, and fibromyalgia. PDs agreed with the GS diagnosis 61% of the time compared to 33% for fellows. Five exam elements not described in the OSCE tool were noted, all involving the neck.
There was no significant difference in the completed number of prespecified 27 exam elements between PDs and fellows but PDs completed a significantly greater number of cervical spine elements and measures of exam technique then fellows, and spent less time on the exam (Table 1). The Hawkins, Neer, belly press, and horn blower’s tests were never performed by any of the PDs.
Conclusion: Exam technique distinguished PDs from fellows most clearly, as did greater attention to exam of the neck for evaluation of shoulder pain. PDs and fellows performed just over half of the exam elements previously described in a shoulder OSCE, and this number did not distinguish the two groups. These results suggest that more emphasis should be placed on exam technique assessment during OSCE examinations in place of performing a greater number of maneuvers
To cite this abstract in AMA style:
Martirossian L, Kalish R, O'Rourke K, Panginikkod S, Kissin E. A Shoulder to Lean On: Differences in Shoulder Examinations Between Rheumatology Educators and Fellows [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/a-shoulder-to-lean-on-differences-in-shoulder-examinations-between-rheumatology-educators-and-fellows/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-shoulder-to-lean-on-differences-in-shoulder-examinations-between-rheumatology-educators-and-fellows/