Session Information
Date: Tuesday, October 23, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster III: Treatment
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Glucocorticoids, anti-malarials and conventional immunosuppressive agents have been the mainstay of therapy for systemic lupus erythematosus (SLE) and lupus nephritis (LN); more recently biologic agents have been introduced for their treatment. We evaluated utilization trends in SLE and LN therapy over the past decade.
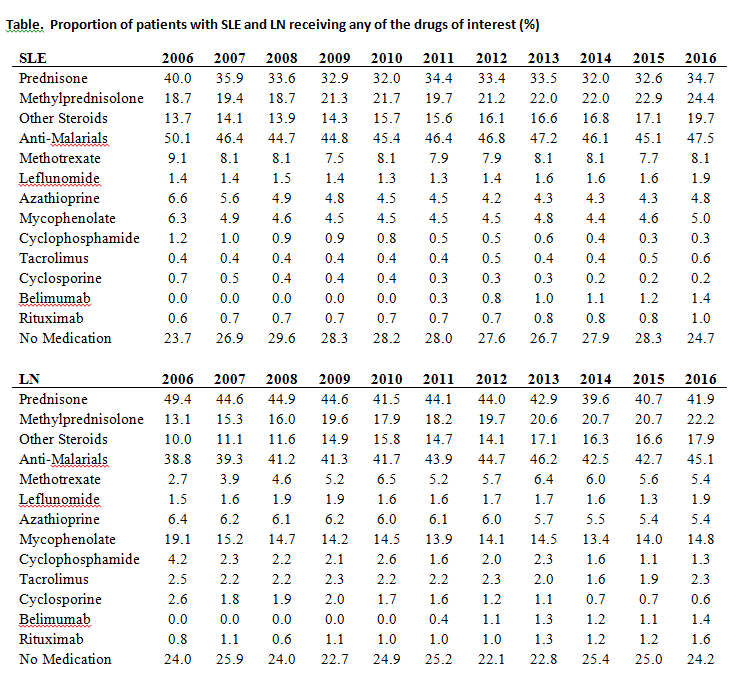
Methods: Using 2006-2016 data from a large administrative database of commercially insured and Medicare Advantage beneficiaries, we identified patients with SLE and a subset of patients with LN based on validated claims-based algorithms. Included patients had at least one year of enrollment in the cohort. We estimated the annual age- and sex- standardized proportion of patients who filled prescriptions for at least one of the drugs of interest (Table).
Results: A total of 30,787 patients with prevalent SLE were identified, of whom 5,267 had LN. Mean age (SD) was 49.3 (14.1) years for SLE and 51.9 (17.2) years for LN. Ninety percent were female, 61.0% White, 17.4% Black, 11.2% Hispanic, 3.0% Asian and 7.0% other/unknown. Use and time trends of therapeutic agents for 2006-2016 are included in the table. Anti-malarials were the most frequently used drug class for both SLE and LN, with some temporal change over the course of the study; 50.1% in 2006 to 47.5% in 2016 for SLE, and 38.8% in 2006 to 45.1% 2016 for LN. Prednisone was the second most frequently used drug, decreasing from 40.0% in 2006 to 34.7% in 2016; use of methylprednisolone and other systemic glucocorticoids increased during that time period. Methotrexate was the most commonly used nonbiologic immunosuppressive drug in SLE (8.0%), while MMF was most frequently prescribed in LN (15.0%), both of which remained stable during the study period. Cyclophosphamide use declined over the last decade for both SLE (1.2% to 0.3% in 2016) and LN (4.2% to 1.3% in 2016). Belimumab was the most commonly used biologic for SLE with a slight uptrend since approval. Rituximab use increased in SLE and was the most commonly used biologic for LN. At any point in time ~24% of the patients were not receiving any of the medications of interest.
Conclusion: Over the past decade, a substantial proportion of patients with SLE and LN continued to receive glucocorticoids. Although the use of prednisone declined, the use of methylprednisolone and other glucocorticoids increased concurrently. The proportion of patients receiving nonbiologic immunosuppressants remained relatively stable for both SLE and LN, however there was a progressive decline in the use of cyclophosphamide. Since 2011 the proportion of patients receiving rituximab is higher than for cyclophosphamide. The increasing use of biologics for SLE and LN, particularly rituximab, which is not currently approved for SLE, highlights the need to clarify their therapeutic role in these diseases.
To cite this abstract in AMA style:
Duarte-Garcia A, Crowson CS, McCoy R, Schilz S, Van Houten H, Sangaralingham L, Chowdhary VR, Amin S, Warrington KJ, Matteson EL, Shah N. Trends in Treatment of Systemic Lupus Erythematosus and Lupus Nephritis: 2006-2016 [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/trends-in-treatment-of-systemic-lupus-erythematosus-and-lupus-nephritis-2006-2016/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trends-in-treatment-of-systemic-lupus-erythematosus-and-lupus-nephritis-2006-2016/