Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: During pregnancy, history of lupus nephritis (LN) has been independently associated with increased risk of adverse maternal and fetal outcomes, which are even more frequent when LN is active at conception. The objective of this study was to analyze the impact of different classes of lupus nephritis (LN) as risk variables for maternal and fetal adverse outcomes in a cohort of pregnant lupus patients.
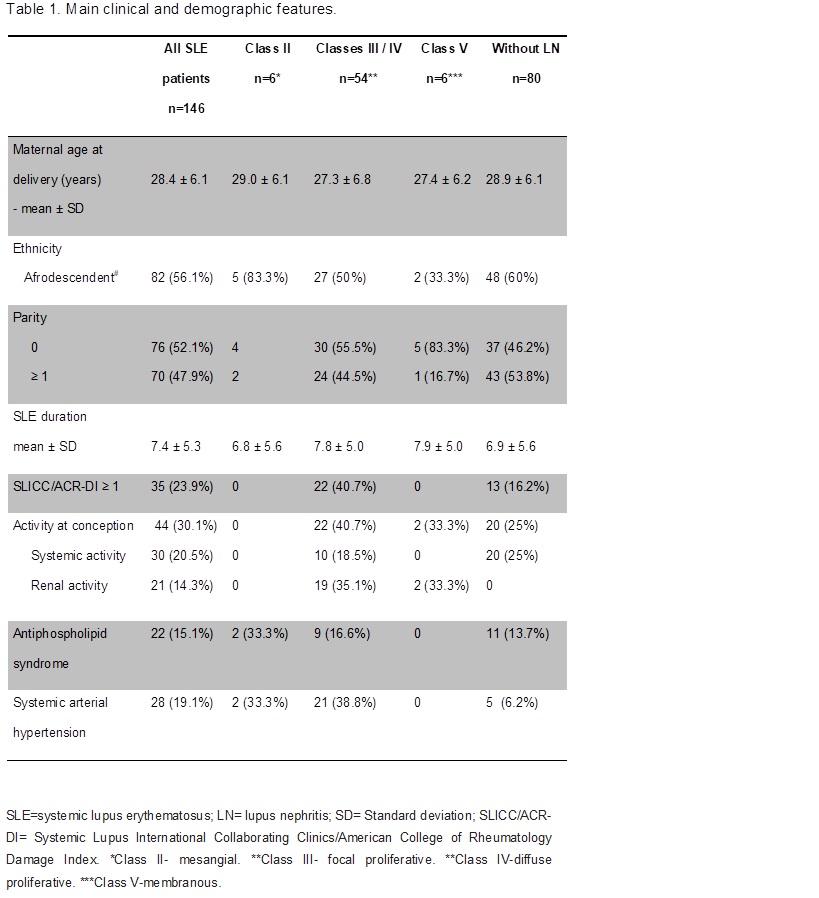
Methods: 146 pregnancies of 136 SLE patients (ACR criteria) were included. Maternal adverse outcomes observed for each nephritis class among LN patients were compared with those without nephritis. Demographic and clinical features of SLE were recorded, including maternal age at delivery, parity and ethnicity, years since the diagnosis of SLE, activity at conception, association with antiphospholipid syndrome, systemic arterial hypertension and permanent damage defined by SLICC/ACR damage index (SDI). Fischer exact test was used for categorized variables and Student’s t test was used for the continuous variables.
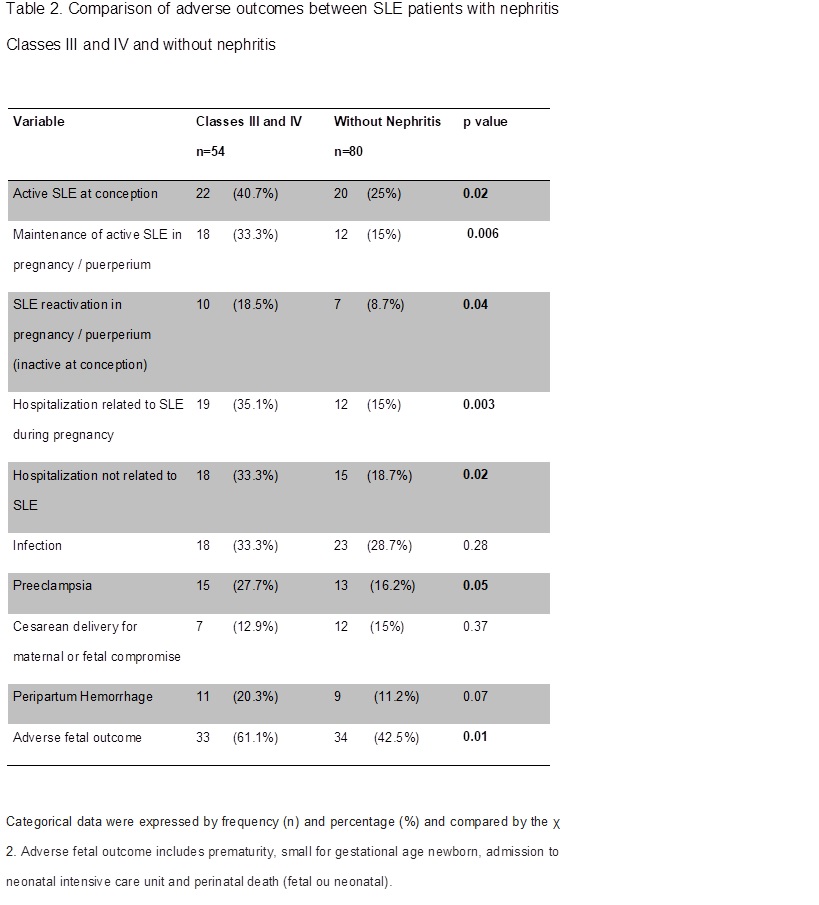
Results: 54 patients had proliferative LN (classes III and IV), 12 had mesangial or membranous LN (classes II and V) and 80 did not have LN. SLE patients with proliferative LN but not those with classes II and V had more frequently SLE activity at conception (p=0.02), flares (p=0.04) or continuous active disease during pregnancy and puerperium (p=0.006), hospitalization for any cause (p=0.003) and due to SLE (p=0.02) and preeclampsia (p=0.05) than patients without nephritis. When classes II and V LN were compared to patients without LN, there were no statistically significant differences in the main outcomes measured. SDI ≥ 1 was more frequent in classes III and IV than among the other patients, even when renal scores were not included. Adverse fetal outcomes such as prematurity, small for gestational age newborns, admission to NICU and perinatal death were more frequent in patients with proliferative LN (61% vs 42.5%; p=0.01), but not with mesangial and membranous LN (41.6% vs 42.5%; p=0.60) when compared to lupus patients without LN.
Conclusion: SLE patients with proliferative nephritis (classes III and IV), but not with classes II or V, have a higher frequency of adverse maternal and fetal outcomes. This is probably due to the major impact of proliferative forms of nephritis on women global heath, which is corroborated by the higher SDI found. These findings suggest that further LN classification beyond the common term nephritis in the context of lupus pregnancy as the impact on maternal and fetal outcomes varies according to histological classes.
To cite this abstract in AMA style:
Costa Rodrigues B, Ignacchiti Lacerda M, Ramires de Jesus G, dos Santos FC, Ramires de Jesus N, Levy RA, Klumb EM. The Impact of Different Classes of Lupus Nephritis on Maternal and Fetal Outcomes [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-different-classes-of-lupus-nephritis-on-maternal-and-fetal-outcomes/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-different-classes-of-lupus-nephritis-on-maternal-and-fetal-outcomes/