Session Information
Date: Sunday, October 21, 2018
Title: 3S082 ACR Abstract: Imaging of Rheumatic Diseases I: MRI & CT (863–868)
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose:
Metacarpal head directly exposed to intra-articular inflammatory milieu, therefore may lead to abnormal bone remodeling (bone loss and new bone formation).
The aims of this study are to investigate the structural (bone erosion and enthesiophyte) and microstructural bone changes in patients with PsA at the second and third metacarpal head (MCH2&3) compared with controls.
Methods:
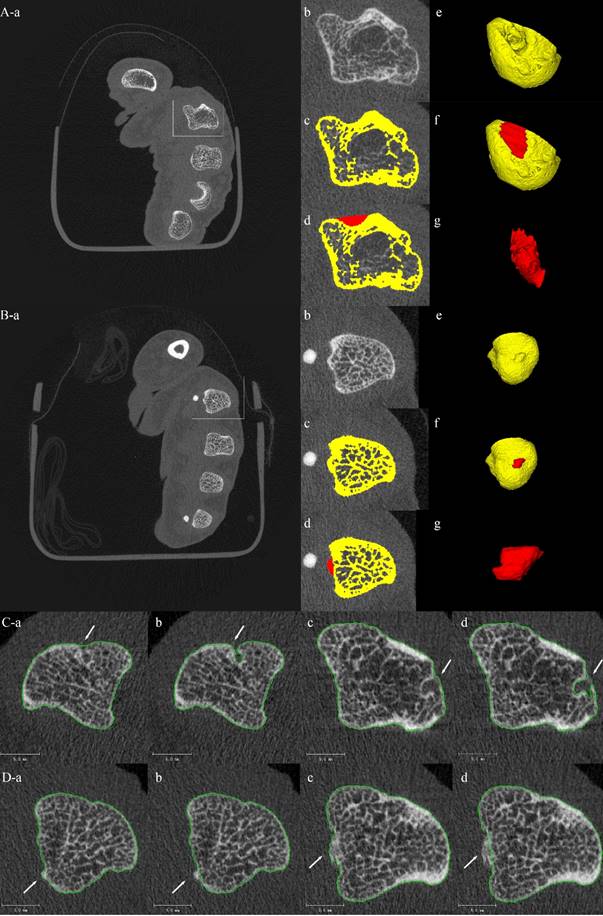
139 subjects (77 PsA, 62 control) underwent high-resolution peripheral quantitative computed tomography (HR-pQCT) scanning at the MCH 2 and 3 and distal radius. Structural and microstructural bone changes at the MCH 2 and 3 were calculated (Figure 1) and compared between PsA patients and healthy controls.
Results:
15 patients with joint destruction were excluded from further analysis. 62 patients with PsA and controls were comparable in age, gender and body mass index (BMI). PsA patients had a significantly increased number (2.4±1.4 vs 1.3±1.1, p<0.001) and total enthesiophytes volume per person (8.75±6.92 vs 4.36±4.90 mm3, p<0.001) compared to controls. Erosion number (2.9±1.2 vs 2.7±1.4, p=0.408) and total erosion volume per person (11.88±7.82 vs 9.64±5.96 mm3, p=0.076) were similar in PsA patients compared with control. Regarding microstructure, PsA patients had a significantly decreased total volumetric bone mineral density (vBMD), cortical vBMD and cortical thickness at the distal radius; while a preferential bone loss at the trabecular compartment at the MCH was noticed compared to control. Regression model in PsA showed that advancing age, a higher BMI and C-reactive protein level were independent explanatory variables associated with a larger erosion volume. In contrast, older age and swollen joint count were independent explanatory variable associated with an increase in enthesiohyte volume.
Conclusion:
Intra-articular trabecular bone loss and entheseal new bone formation was more prevalent in the MCH of patients with PsA.
Disclosures: This study has been partly presented at EULAR2018.
To cite this abstract in AMA style:
Wu D, Griffith JF, Lam SHM, Yue J, Wong P, Shi L, Li E, Cheng IT, Li TK, Zhu TY, Hung VW, Qin L, Tam LS. Structural and Microstructural Intraarticular Bone Changes at the Metacarpal Heads in Patients with Psoriatic Arthritis Compared to Controls: A HR-pQCT Study [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/structural-and-microstructural-intraarticular-bone-changes-at-the-metacarpal-heads-in-patients-with-psoriatic-arthritis-compared-to-controls-a-hr-pqct-study/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/structural-and-microstructural-intraarticular-bone-changes-at-the-metacarpal-heads-in-patients-with-psoriatic-arthritis-compared-to-controls-a-hr-pqct-study/