Session Information
Date: Wednesday, November 8, 2017
Title: Osteoarthritis – Clinical Aspects II: Structural Progression and Incidence
Session Type: ACR Concurrent Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose: Osteophytes are formed through reactivation of endochondral ossification. In adults, reactivation of endochondral ossification may occur in the context of fracture repair. As yet, the rationale for the genesis of osteophytes in osteoarthritis (OA) remains unclear. We investigated whether bone marrow lesions (BMLs) (representing subchondral remodeling due to increased loading) and inflammation (assessed as effusion-synovitis on non-contrast-enhanced MRI) were associated with the presence and progression of osteophytes in OA knees.
Methods: We analyzed data from 600 participants included in the FNIH Biomarkers study within the Osteoarthritis Initiative. Osteophytes and BMLs were scored according to size (0-3) on MRI in the medial and lateral femur and tibia, and effusion-synovitis was scored in the whole knee according to severity (0-3, where 0 means absent) using the MRI OA Knee Score (MOAKS). BMLs and effusion-synovitis were considered present when a score ≥ 1 for each feature was given. Osteophyte severity was categorized into grades 0 (absent), 1 (small) and 2-3 (medium to large). We examined the cross-sectional and longitudinal relation between the baseline presence of BMLs and effusion-synovitis to osteophyte severity and progression (increase in size in ≥ 1 grade) in each joint compartment on MRI over 24 months. Ordinal regression was used for the cross-sectional analysis and binary logistic regression for the longitudinal analysis adjusted for covariates. We assessed the interaction effect between BMLs and knee alignment, measured by goniometer on physical examination (neutral, varus or valgus), using interaction terms.
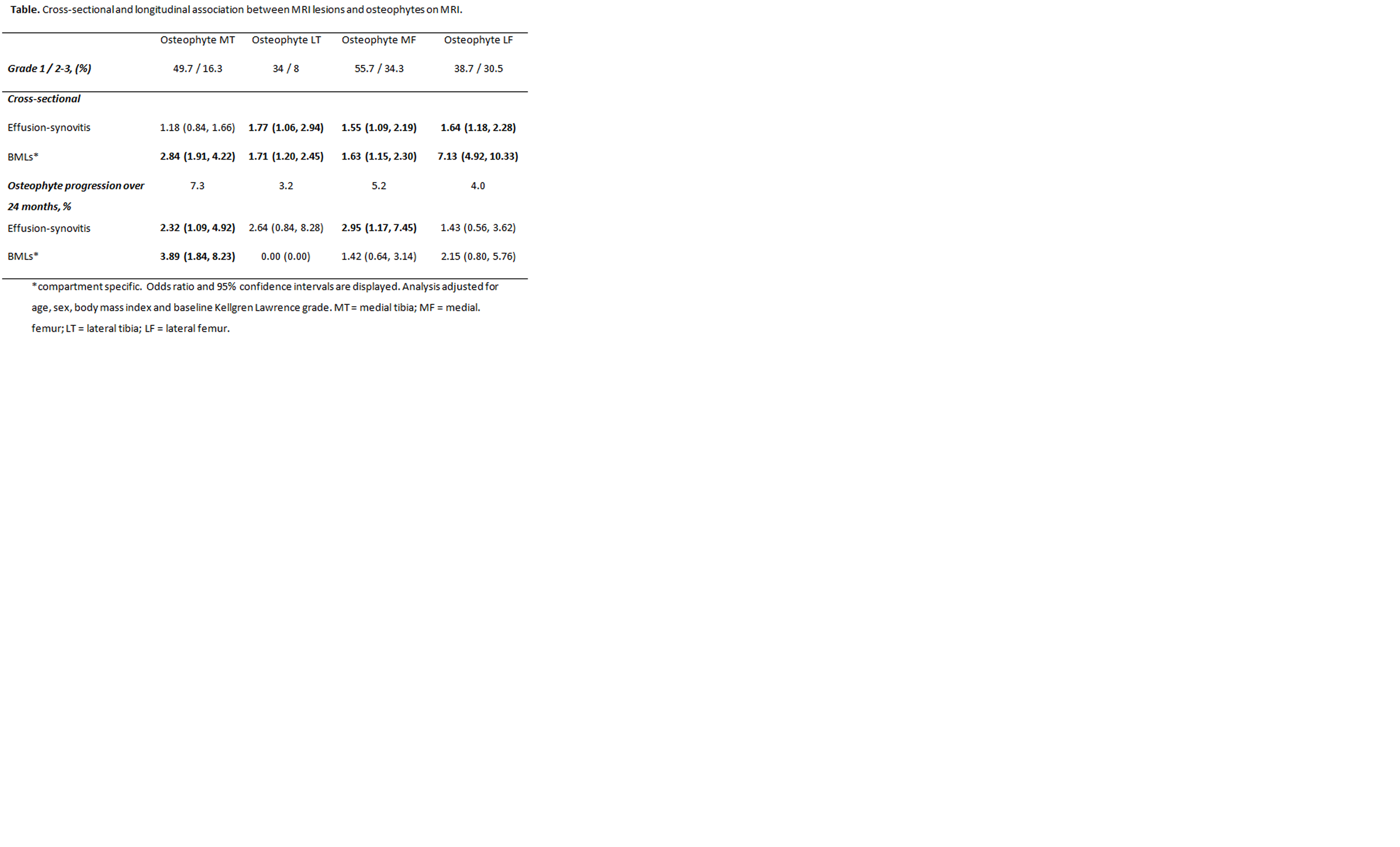
Results: At baseline, BMLs were present in 10.8% to 53.3% depending on the knee compartment and effusion-synovitis was present in 61% of the knees. Presence of BMLs was strongly associated with baseline osteophytes in all four knee compartments (Table), with odds ratios (OR) ranging from 1.63 (95% confidence interval [CI] 1.15, 2.30) in the medial femur to 7.13 (4.92, 10.93) in the lateral femur. Presence of effusion-synovitis was also associated with osteophytes, except in the medial tibia. At baseline, the interaction analysis showed no effect of alignment in the association between BMLs and osteophytes. Over 24 months, osteophyte progression mostly occurred in the medial tibia (7.3%) and was strongly associated with the presence of baseline BMLs in the same joint compartment (OR 3.89 [1.84, 8.23]). Baseline effusion-synovitis was also associated with an increase in osteophyte size in the medial femur and tibia.
Conclusion: Bone marrow lesions were strongly associated with the presence of osteophytes and with osteophyte progression on MRI over 24 months. Although inflammation may also play a role in the development of osteophytes, BMLs appear to be more strongly related to the reactivation of endochondral ossification process.
To cite this abstract in AMA style:
Deveza L, Teoh L, Ochoa-Albiztegui E, Guermazi A, Roemer F, Hunter D. Do Bone Marrow Lesions Reactivate Endochondral Ossification Leading to Osteophyte Genesis? Data from the Osteoarthritis Initiative [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/do-bone-marrow-lesions-reactivate-endochondral-ossification-leading-to-osteophyte-genesis-data-from-the-osteoarthritis-initiative/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/do-bone-marrow-lesions-reactivate-endochondral-ossification-leading-to-osteophyte-genesis-data-from-the-osteoarthritis-initiative/