Session Information
Date: Tuesday, November 7, 2017
Title: Spondyloarthropathies and Psoriatic Arthritis – Clinical Aspects and Treatment IV
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Title: Clinical Evolution of Patients with Inflammatory Back Pain: a Population-Based Longitudinal Cohort Study
Authors: Runsheng Wang1, Cynthia Crowson2, Kerry Wright2, Michael Ward3
1. Columbia University Medical Center, New York, NY
2. Mayo Clinic, Rochester, MN
3. NIH/NIAMS, Bethesda, MD
Background/Purpose: Inflammatory back pain (IBP) is an early manifestation and a key feature of spondyloarthritis (SpA). However the natural history of IBP has not been well defined. Significant differences exist between the prevalence of IBP (3-6%) and prevalence of SpA (0.5-1%), suggesting either that IBP often resolves or is due to conditions other than SpA. The objective of this study was to investigate the long-term outcomes of IBP, and clinical predictors of progression to SpA.
Methods: A population-based cohort of patients with incident IBP in 2000-2003 among residents of a geographically defined area was established retrospectively. Using diagnostic codes for back pain on clinic visits, we screened and validated the presence of new-onset IBP among patients age 16 to 35 via manual medical record review. Verified patients either met the Calin, Berlin, or ASAS criteria, or were considered by their treating rheumatologist to have IBP. We collected data on clinical SpA features, HLA-B27 status, inflammatory markers, and imaging, and followed their outcomes until July 2016. Aalen-Johansen methods (a multistate generalization of cumulative incidence with adjustment for competing risks) were used to examine their evolution to one of 3 outcomes: progression to SpA, progression to a non-SpA diagnosis, or resolution of back pain. Recursive partitioning with a time to event outcome was used to identify predictors for progression to SpA.
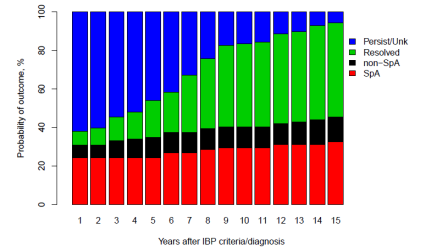
Results: After screening 5304 patients, we identified 124 subjects with new-onset IBP from 2000 to 2003. After a median of 13.2 years of follow up, progression to SpA occurred in 39 patients (Figure). The probability of having SpA at 5, 10, 15 years was 24%, 30%, and 33%, respectively. In almost half of the patients, their IBP resolved during follow up. Progression was seen in 85% of 13 patients with a history of uveitis, and 26% of 111 patients without history of uveitis by 15 years after IBP incidence. Among those without a history of uveitis, progression was seen in 32% of men and 14% of women by 15 years.
Conclusion: Less than 1/3 of patients with new-onset IBP progress to SpA over more than a decade of follow up, while many resolve. History of uveitis is the most important predictor for progression.
Figure. Progression from IBP to SpA, non-SpA conditions, back pain resolved, and persistent back pain.
To cite this abstract in AMA style:
Wang R, Crowson CS, Wright K, Ward M. Clinical Evolution of Patients with Inflammatory Back Pain: A Population-Based Longitudinal Cohort Study [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/clinical-evolution-of-patients-with-inflammatory-back-pain-a-population-based-longitudinal-cohort-study/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-evolution-of-patients-with-inflammatory-back-pain-a-population-based-longitudinal-cohort-study/