Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The antimalarial drug hydroxychloroquine (HCQ) has been used for decades to treat various rheumatic diseases including systemic lupus erythematosus (SLE). The efficacy of HCQ in lupus is well-demonstrated, and leads to a decreased number of lupus flares. Although multiple mechanisms have been proposed for HCQ, the systemic immunologic effects of HCQ treatment still remains ill-defined in human lupus and may help elucidate the immune mechanisms of HCQ in SLE.
Methods: SLE patients receiving HCQ (n=9) or not receiving HCQ (n=9) were matched and assessed in a cross-sectional design. Single-cell analysis of surface markers were completed by mass cytometry on PBMCs and cellular heterogeneity was visualized using viSNE and manual gating in Cytobank. Further, phospho-specific flow cytometry was used to measure basal levels of pERK, pPLCγ2, pSTAT5 and p38 and expression following CD3/CD28 (TCR) and anti-IgG and IgM (BCR) stimulation. Soluble mediator levels in plasma were assessed using a 51-plex (Affymetrix) and by ELISA (eBioscience). All SLE patients met ACR criteria for SLE classification.
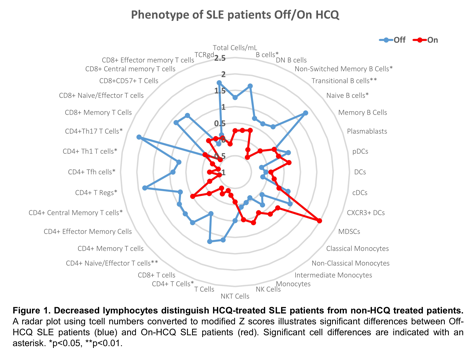
Results: In PBMCs of SLE patients taking HCQ, there was a small non-significant trend towards fewer total cells/mL compared to SLE patients not receiving HCQ (p=0.1200) (Figure 1). There was a significant reduction in the number of B cells (p=0.0269) and CD4+ T Cells (p=0.0124), most significantly transitional B cells (p=0.0053) and effector T cells (p=0.0039) (Th1-type, Th17-type, and Tfh-type) in HCQ patients compared to non-HCQ patients (Figure 1). Cell activation was also reduced in SLE patients receiving HCQ with lower expression of HLA-DR and CD38 on B cells, IL-2 receptor and CCR6 on T cells, and CD86 expression in dendritic cells (p<0.05). Plasma soluble mediators produced primarily by monocyte, platelet and endothelial cells were significantly reduced in patients receiving HCQ, namely PDGF-BB (p=0.0009), MCP-1 (p=0.0041), PAI-1 (p=0.0114), sEselectin (p=0.0118), resistin (p=0.0360) and IL-7 (p=0.0380). No significant differences were observed in TCR and BCR signaling following stimulation, but reduced levels of PLCg in CD4+ effector T cells were found in SLE patients receiving HCQ following BCR stimulation (p=0.0275).
Conclusion: Our results indicate that SLE patients on HCQ have reductions in circulating lymphocytes, HLA-DR expression on antigen-presenting cells, and monocyte and platelet derived soluble mediators compared to patients off HCQ. In addition, reduced T cell signaling following B cell stimulation suggests that the effects of HCQ on T cells may be a result of altered antigen presentation and reduced IL-7 levels. Together these data provide potential insights into HCQ mechanisms of action in SLE patients, while suggesting use lowers the risk of thrombotic events by reducing platelet activation.
To cite this abstract in AMA style:
Slight-Webb S, Lu R, Chen H, Maecker HT, Utz PJ, Guthridge JM, James JA. Hydroxychloroquine Use Is Associated with Decreased Dendritic Cell Activation and Thrombolytic Factors in SLE Patients [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/hydroxychloroquine-use-is-associated-with-decreased-dendritic-cell-activation-and-thrombolytic-factors-in-sle-patients/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hydroxychloroquine-use-is-associated-with-decreased-dendritic-cell-activation-and-thrombolytic-factors-in-sle-patients/