Session Information
Date: Tuesday, November 7, 2017
Title: Pediatric Rheumatology – Clinical and Therapeutic Aspects Poster III: Juvenile Arthritis
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Relatively little is known about the epidemiology of juvenile psoriatic arthritis (PsA), including risk factors for development of PsA among children with psoriasis. It is also unknown whether children with PsA are at increased risk of cardiovascular and metabolic disease, similar to adults.
Methods: We conducted a retrospective cohort study of children with incident psoriasis and PsA using the Clinformatics TM DataMart (OptumInsight, Eden Prairie, MD), a de-identified administrative claims database. All incident psoriasis patients had ≥1 ICD-9 code for psoriasis and PsA patients had ≥ 1 ICD-9 code for PsA or psoriasis and arthritis. The index date was the date of the first ICD-9 code for the diagnosis of psoriasis or PsA. Patients were required to be continuously enrolled for 6 months before and 12 months after the index date. Controls were matched on age, sex, and date of psoriasis or arthritis diagnosis at a 10:1 ratio. Cox proportional hazard regression was performed to assess the risk of developing arthritis in children with psoriasis over time. Incidence rate ratios were used to compare the relative frequency of cardiovascular and metabolic co-morbid diagnoses.
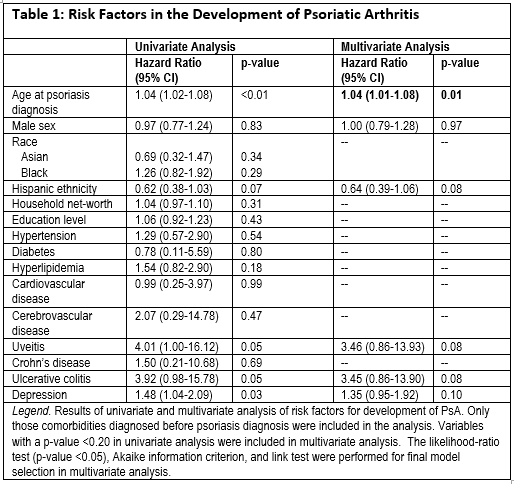
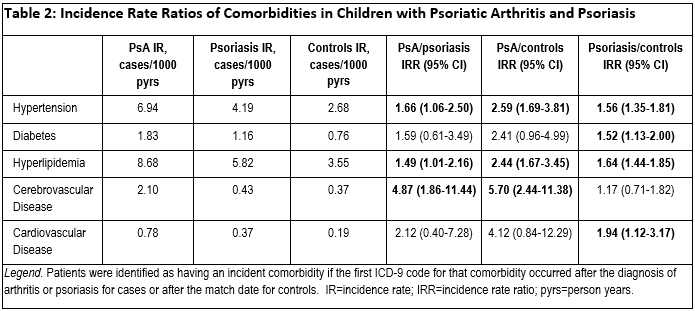
Results: We identified 1,012 children with PsA, 14,610 with psoriasis, and 203,907 controls. The median time of continuous enrollment was 3.0 years (IQR 1.9-4.9). Median ages at the first diagnoses of PsA and psoriasis were 12 and 10 years, respectively. 56% and 53% of children with PsA and psoriasis were female. Amongst those children who had both psoriasis and arthritis, approximately 37% developed psoriasis first. Median time to development of arthritis after psoriasis diagnosis was 1.8 years (IQR 0.4-2.8). Older age was associated with a significantly increased risk of developing arthritis in children with psoriasis (Table 1). There was a trend towards increased risk of arthritis in psoriasis patients with ulcerative colitis and uveitis, albeit statistically insignificant. Children with psoriatic arthritis had a significantly increased incidence of hypertension, hyperlipidemia, and cerebrovascular disease compared to healthy controls (Table 2).
Conclusion: Older age was a risk factor for PsA among children with psoriasis. Similar to adults, PsA was associated with a higher risk of developing metabolic and cerebrovascular disease in children.
To cite this abstract in AMA style:
Manos CK, Xiao R, Brandon TG, Ogdie A, Weiss PF. Risk Factors for Arthritis and the Development of Comorbid Cardiovascular and Metabolic Disease in Children with Psoriasis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/risk-factors-for-arthritis-and-the-development-of-comorbid-cardiovascular-and-metabolic-disease-in-children-with-psoriasis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-for-arthritis-and-the-development-of-comorbid-cardiovascular-and-metabolic-disease-in-children-with-psoriasis/