Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Juvenile idiopathic inflammatory myopathies (JIIM) are rare, autoimmune chronic muscle diseases of childhood with significant potential long-term morbidity. In this study we investigate associations of clinical and demographic factors with long-term outcomes in a referral population of patients with JIIM who are currently adults.
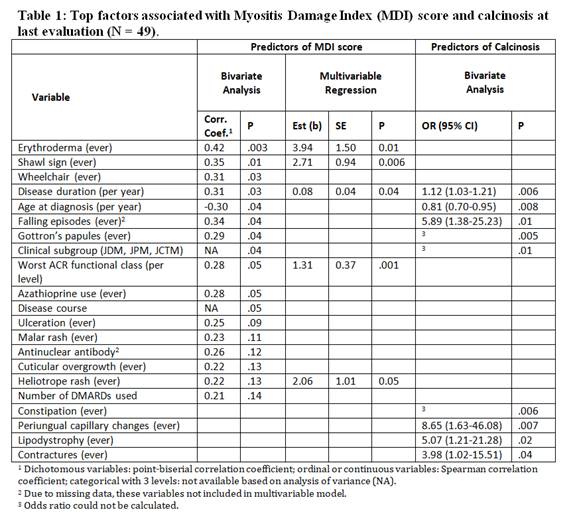
Methods: Adults with JIIM were assessed at two referral centers between 1994 and 2016. Bivariate analysis was used to test for associations of 94 clinical, demographic, and laboratory factors with two long-term outcomes: a higher Myositis Damage Index (MDI) and the presence of calcinosis on last evaluation. A multivariable regression model for MDI used backwards selection on factors with statistically significant associations (p < .15) in bivariate analysis.
Results: Forty-nine patients with probable or definite JIIM (37 dermatomyositis, 5 polymyositis, 7 overlapping myositis) had a median age of 24 years [IQR 19, 28], and median follow-up period of 12 years after diagnosis [IQR 5, 20]; 59% were Caucasian and 82% were female; 63% had a chronic, 31% a polycyclic, and 6% a monocyclic illness course. Damage was present in 96%, with a median MDI score of 6 [IQR 3, 9]. Cutaneous (80%) and muscle (78%) damage were most frequent and most severe (median score 2 [IQR 1, 3] for both) among the MDI organ systems. Calcinosis was present in 55% of patients. Of the 94 potential predictors, 17 were significantly (p < 0.15) associated with total MDI score and 11 were significantly (p < 0.05) associated with the presence of calcinosis (Table). All selected variables in the multivariable model were independently associated with a higher MDI score: erythroderma, shawl sign, disease duration, worst ACR functional class, and heliotrope rash. Several factors were strongly associated with calcinosis in bivariate analysis including disease duration, younger age at diagnosis, falling episodes, Gottron’s papules, clinical subgroup JDM, constipation, periungual capillary changes, lipodystrophy, and contractures (Table). The multivariable logistic regression model for calcinosis did not converge due to the small sample size.
Conclusion: This is one of the largest cohorts of patients with JIIM evaluated for long-term outcomes into adulthood. We were able to identify multiple clinical factors associated with long-term damage and calcinosis when JIIM patients become of adult age, which included specific cutaneous and musculoskeletal features.
To cite this abstract in AMA style:
Tsaltskan V, Aldous A, Serafi S, Sami H, Mamyrova G, Miller FW, Simmens S, Curiel R, Jones OY, Rider LG. Clinical Factors Associated with Long-Term Damage and Calcinosis in an Adult-Age Referral Population of Juvenile Myositis Patients [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/clinical-factors-associated-with-long-term-damage-and-calcinosis-in-an-adult-age-referral-population-of-juvenile-myositis-patients/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-factors-associated-with-long-term-damage-and-calcinosis-in-an-adult-age-referral-population-of-juvenile-myositis-patients/