Session Information
Date: Monday, November 6, 2017
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
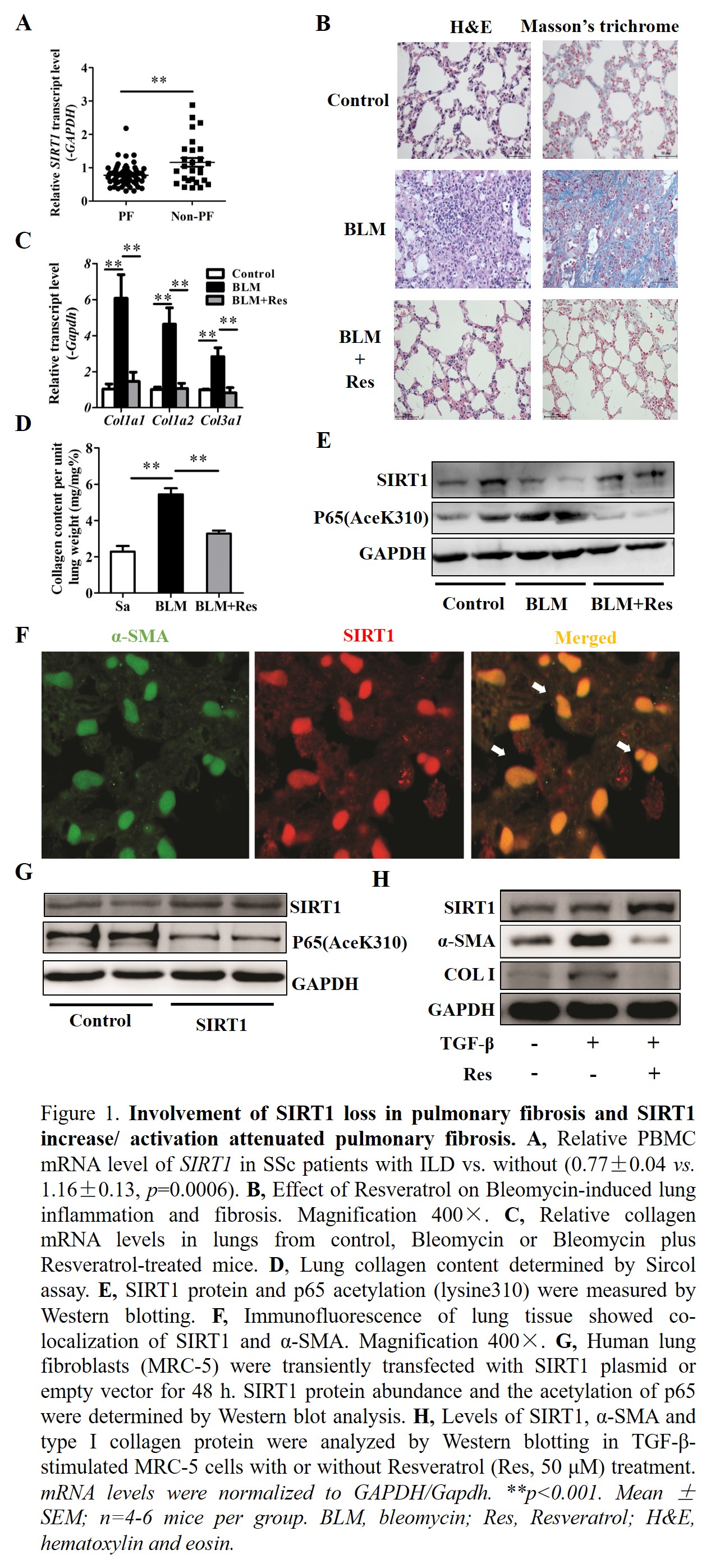
Interstitial lung disease (ILD) is the leading cause of death in systemic sclerosis (SSc). Sirtuin1 (SIRT1) is a deacetylase with known anti-inflammatory and anti-fibrotic activity; the role of SIRT1 in SSc-ILD is unclear.
Methods:
Total RNA was extracted from peripheral blood mononuclear cells (PBMCs) isolated from SSc patients (n=86). In in vivo studies, mice were administered intratracheal bleomycin (BLM) (2.5 U/kg) to induce pulmonary fibrosis. Resveratrol (Res, 25 mg/kg) was fed daily from the third day before BLM instillation for the Prevention Study or 10 days post-BLM for the Treatment Study. Histological analysis was performed to assess lung inflammation/fibrosis. Immunofluorescence staining was used to identify the cell type expressing SIRT1. For in vitro studies, human lung fibroblasts were treated with TNF-aerfa (10 ng/ml)/TGF-beita (10 ng/ml) with or without SIRT1 activator (Res, 50 uM)/plasmid or inhibitor (Nicotinamide, 20 mM) /siRNA. Real-time PCR or Western blotting was used to measure mRNA or protein level (including SIRT1, P65 acetylation, Smad3 and mTOR phosphorylation).
Results:
The expression of SIRT1 in PBMCs of SSc patients with ILD (n=59) was significantly lower than that in SSc patients without ILD (n=27) (0.77¡À0.04 vs. 1.16¡À0.13, Fig.1A). Further analysis found the decreased expression of SIRT1 was correlated with dcSSc and the presence of ATA. In the in vivo studies, SIRT1 activation with Res reduced lung inflammation and fibrosis when it was administered either as prevention or as therapy, as evidencing by histological analysis (Fig.1B), decreased inflammatory gene expression and cytokine production as well as collagen production (mRNA level: Col1a1 reduced 72.5%, Col1a2 reduced 76.7% and Col3a1 reduced 72.3%; collagen content reduced 39.8%. Fig.1C-D). SIRT1 was expressed in aerfa-SMA+ myofibroblasts in mouse lung tissue, indicating an inhibitory effect of SIRT1 on myofibroblasts (Fig.1F). Moreover, SIRT1 activation or overexpression inhibited TNF-aerfa-induced inflammatory responses in vitro while depletion of SIRT1 in fibroblasts enhanced inflammation; and these effects were related to the decrease or increase in the acetylation of NF-kappaB, respectively (Fig.1G). These results were consistent with data of our in vivo experiments that Res treatment increased SIRT1 expression level and activity and blunted NF-kappaB signaling (Fig.1E). In addition, SIRT1 activation or exogenous overexpression inhibited collagen production in vitro (Fig.1H) via inactivation of TGF-beita/Smad3 and mTOR signaling.
Conclusion:
SIRT1 loss contributed to BLM induced pulmonary fibrosis and may play a role in SSc-ILD, while SIRT1 activation was effective for both the early (inflammatory) and late (fibrotic) stages of BLM induced fibrosis. Thus, SIRT1 could be a promising therapeutic target in the treatment of SSc-ILD.
To cite this abstract in AMA style:
Chu H, Jiang S, Liu Q, Qian F, Zhou X, Mayes MD, Jin L, Wang J. SIRT1 May Protect Against Systemic Sclerosis-Related Pulmonary Fibrosis By Decreasing Pro-Inflammatory and Pro-Fibrotic Processes [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/sirt1-may-protect-against-systemic-sclerosis-related-pulmonary-fibrosis-by-decreasing-pro-inflammatory-and-pro-fibrotic-processes/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sirt1-may-protect-against-systemic-sclerosis-related-pulmonary-fibrosis-by-decreasing-pro-inflammatory-and-pro-fibrotic-processes/