Session Information
Date: Sunday, November 5, 2017
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Hepatitis B infection remains a significant public health challenge, particularly for patients on chronic immunosuppressive therapy, due to a considerable mortality risk associated with hepatitis B reactivation. Serologic screening for immunocompromised patients should include hepatitis B surface antibodies (anti-HBsAb) to assess for immunity, hepatitis B core antibodies (anti-HBcAb) and hepatitis B surface antigen (HBsAg) to evaluate for acute or chronic infection. Our primary aim was to determine the burden of non-immunity against hepatitis B, provide insight into factors leading to lack of immunity against hepatitis B and establish the basis for the need for universal screening of these patients. Secondarily, we determined serologic response to a single hepatitis B vaccination booster.
Methods:
Subjects are patients seen at the rheumatology and inflammatory bowel disease (IBD) clinics who are immunocompromised. We use a clinical algorithm as part of standard practice to check hepatitis B serology in immunocompromised patients, offer a booster vaccination if needed, and then repeat serology to determine the response. The results of anti-HBsAb are reported as positive, negative or indeterminate. Immunity is defined as a positive result for anti-HBsAb. An indeterminate or negative result for anti-HBsAb is non-immune. A retrospective chart review was performed to collect demographic and clinical factors as well as serology results. Descriptive statistics were calculated for all variables. R software was used to perform all analyses. For continuous variables, mean and standard deviation are reported, and comparisons were calculated using two-sample t-tests. For categorical variables, frequency and percentage are reported, and comparisons were calculated using chi-square tests.
Results:
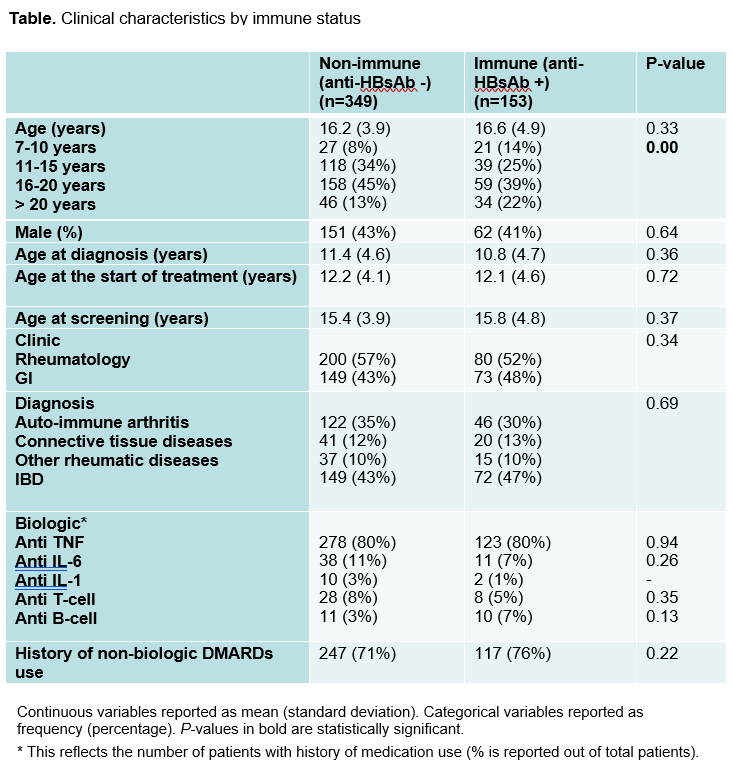
A total of 502 patient charts of immunocompromised patients were reviewed, 280 rheumatology and 222 IBD. Out of the 502 patients, 70% were non-immune (anti-HBsAb negative/indeterminate) (see Table). The highest portion of non-immune patients were those between the ages of 16-20 years (p=0.005) There was no clinically significant difference between immune and non-immune patients with regards to diagnosis (p=0.69), age at the start of treatment (p=0.72) or type of medications. A total of 196 non-immune patients received a booster dose of hepatitis B vaccine and 61 (72%) of those re-screened developed a positive anti-HBsAB. Of note, one patient was identified with a previously unknown chronic hepatitis B infection (anti-HBcAb positive).
Conclusion:
A majority of patients had non-immune hepatitis B serology. Lack of serologic immunity is highest at 16-20 years. A majority of patients developed positive anti-HBsAb following booster vaccination. Results support serologic screening for hepatitis B in immunocompromised patients.
To cite this abstract in AMA style:
Aljaberi N, Smitherman EA, Ghulam E, Watts A, Dykes DM, Huggins JL. Protection Against Hepatitis B in Immunocompromised Pediatric Rheumatology and Gastroenterology Patients [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/protection-against-hepatitis-b-in-immunocompromised-pediatric-rheumatology-and-gastroenterology-patients/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/protection-against-hepatitis-b-in-immunocompromised-pediatric-rheumatology-and-gastroenterology-patients/