Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Repository corticotropin injection (RCI) may produce anti-inflammatory and immune-modulatory effects. This study examined the demographics of those who used RCI and the trends in medication use, specifically prednisone, after RCI initiation.
Methods: This retrospective analysis of the Symphony Health Solutions Patient Transactional Dataset from 2008 to 2015 included patients with at least 1 claim for RA, SLE, or DM/PM, and any use of RCI. Patients with claims for non-rheumatologic conditions that may also be treated by RCI, namely, multiple sclerosis and proteinuria, were excluded. Demographics, patterns of RCI use, and concomitant medications (corticosteroids [CS], biologics, NSAIDs, and DMARDs) were reported. Patients were followed for concomitant medication use from 2 years prior to and 1 year after RCI initiation. Paired two-tailed t-test was used to calculate the p values for the use of each drug class before/after RCI initiation.
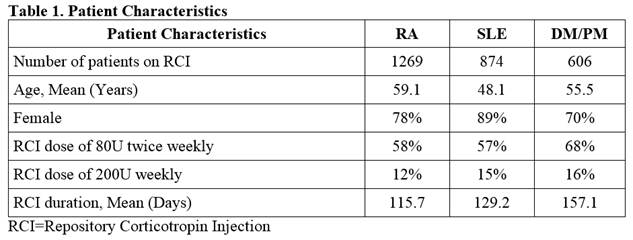
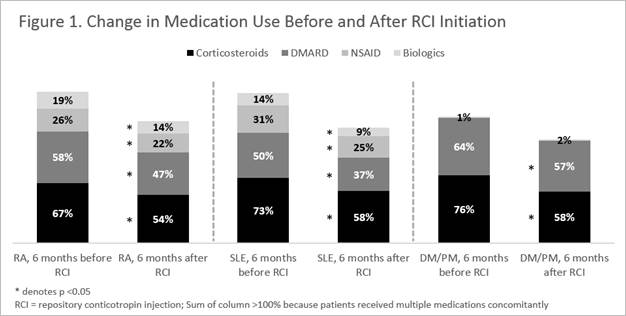
Results: Out of 2.7 million rheumatologic patients in the database over 6 years, there were 2,749 patients who used RCI – 1269 RA patients, 874 SLE patients, and 606 with DM/PM (Table 1). SLE patients were younger than RA and DM/PM patients, and most of the patients were female for all 3 conditions. Majority of patients received 80U of RCI twice weekly. The study identified 504 RA, 322 SLE, and 222 DM/PM patients with sufficient follow up time to evaluate concomitant medication use. For all 3 conditions, the proportions of patients who used any CS were significantly lower after RCI initiation: reduced from 67% pre-index to 54% post-index for RA, from 73% to 58% for SLE, and from 76% to 58% for DM/PM (p < 0.05 for all comparisons, Figure 1). Proportions of patients on biologics and DMARDs were also significantly lowered after RCI initiation. In Figure 2, among patients who had taken CS consistently 24 weeks before RCI initiation, dose reductions were statistically significant for RA (28%), and trended lower without statistical significance for SLE (25%) and DM/PM (25%). Limitation of the retrospective analysis include uncertainties in diagnosis, medication use, and factors influencing medication changes.
Conclusion: This claims-based study of patients with RA, SLE, and DM/PM indicated that RCI use may be associated with significant reductions in CS requirements.
To cite this abstract in AMA style:
Myung G, Nelson W, McMahon MA. Effects of Repository Corticotropin Injection on Medication Use in Patients with Rheumatologic Conditions: A Claims Data Study [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/effects-of-repository-corticotropin-injection-on-medication-use-in-patients-with-rheumatologic-conditions-a-claims-data-study/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effects-of-repository-corticotropin-injection-on-medication-use-in-patients-with-rheumatologic-conditions-a-claims-data-study/