Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Obesity has become alarmingly common over the past four decades in the U.S., with a notable rise in obesity prevalence starting in the late 1980s. Obesity is related to increased risk of several autoimmune diseases, likely via generation of inflammatory adipokines, but prior studies have not evaluated obesity as a risk factor for SLE. We aimed to prospectively evaluate whether obesity is associated with increased SLE risk, particularly during the years in which obesity prevalence was rising most drastically.
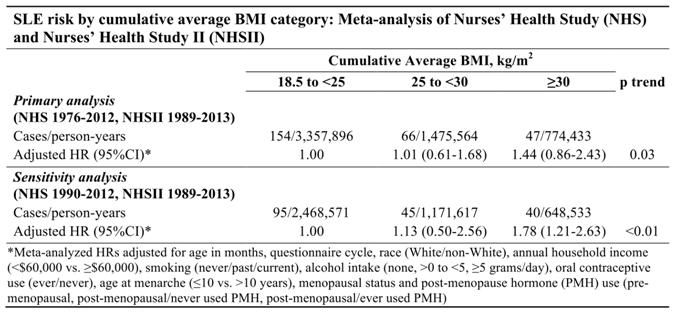
Methods: We conducted a prospective cohort study of women in the U.S. Nurses’ Health Studies (NHS, 1976-2012, aged 30-55 at baseline; NHSII, 1989-2013, aged 25-42 at baseline). Incident SLE was confirmed by ACR 1997 criteria. Body mass index (BMI, kg/m2) was reported at baseline and on biennial questionnaires. We excluded women who did not report BMI at baseline. Cumulative average BMI category, updated every two years, was the primary exposure: 18.5 to <25 (normal [reference]), 25 to <30 (overweight), ≥30 (obese). Cox proportional hazards models estimated HRs (95% CIs) for SLE by cumulative average BMI category, adjusting for time-varying age, race, smoking, alcohol intake, household income, age at menarche, oral contraceptive use, menopausal status and post-menopause hormone use. Analyses were conducted separately in each cohort, and results were meta-analyzed with a DerSimonian-Laird random effects model. We performed a median trend test for SLE risk across increasing BMI categories. In secondary analyses, follow-up started in 1988 (NHS)/1989 (NHSII) when obesity prevalence in the U.S. was increasing most dramatically.
Results: We identified 154 SLE cases in NHS and 113 cases in NHSII. Obesity was present at enrollment in 8.4% (NHS) and 11.8% (NHSII). Mean age at enrollment was 42.7 years (SD 7.1) in NHS and 34.4 years (SD 4.6) in NHSII. 92% of subjects were White in each cohort. At SLE diagnosis, 46.1% (NHS) and 61.1% (NHSII) were anti-dsDNA positive. Obesity was significantly associated with SLE risk in NHSII (HR 1.86, 95% CI [1.17-2.94], p trend 0.02), but did not increase SLE risk in NHS (HR 1.09, 95% CI [0.64-1.84], p trend 0.47). Meta-analysis of NHS+NHSII revealed a significant trend for increased SLE risk by increasing BMI category (p trend 0.03) (Table). When follow-up started in the late 1980s, meta-analysis of NHS+NHSII revealed increased SLE risk among obese women (HR 1.78, 95% CI 1.21-2.63, p trend <0.01).
Conclusion: We observed a significant risk of SLE among obese women in NHSII, which started enrollment later than NHS. Obese women were at 78% elevated risk of developing SLE when follow-up started in both cohorts in the late 1980s, suggesting that secular trends in obesity prevalence were associated with increased SLE risk.
To cite this abstract in AMA style:
Tedeschi SK, Barbhaiya M, Lu B, Malspeis S, Sparks JA, Karlson EW, Willett WC, Costenbader KH. Obesity and the Risk of Systemic Lupus Erythematosus in the Nurses’ Health Studies [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/obesity-and-the-risk-of-systemic-lupus-erythematosus-in-the-nurses-health-studies/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/obesity-and-the-risk-of-systemic-lupus-erythematosus-in-the-nurses-health-studies/