Session Information
Date: Tuesday, November 10, 2015
Title: Systemic Sclerosis, Fibrosing Syndromes and Raynaud's - Clinical Aspects and Therapeutics Poster III
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: In patients with
connective tissue disease (CTD), especially systemic sclerosis (SSc), several
mechanisms have been implicated for the development of pulmonary hypertension
(PH), including pulmonary arterial hypertension (PAH), PH with interstitial
lung disease (PH-ILD) and PH with left heart disease (PH-LHD). The
combination of such different mechanisms lead to the complexity of pathogenesis
that might possibly result in less efficacy of combination therapy using PAH-specific
drugs (CoTpy) for survival in PH-CTD than in idiopathic PAH. The present
study therefore aimed to analyze the factors that influence the effect of CoTpy
on survival of PH-CTD.
Methods: We performed a retrospective-cohort
study of 118 patients with PH-CTD, including 56 SSc, 29 MCTD or 24 SLE patients,
who were followed up between January 1980 and March 2015 in our hospital.
PH was diagnosed based on heart catheterization (HC). Patients with PH-ILD
had been confirmed to have ILD on chest CT scan. Patients with PH-LHD had
been confirmed to have LHD by HC or biopsy. There were 97 PAH, 47 PH-ILD and
9 PH-LHD patients. Our CoTpy strategy for PH intended to achieve the
following goals: 1) improvement in WHO-functional class and 2) reduction of serum
BNP level of less than 100 pg/ml, based on our previous study as well as on the
results demonstrated by Hoeper et. al, (Eur Respir J 2005; 26: 858–863).
The PAH-specific drugs, including bosentan, ambrisentan, sildenafil, tadalafil,
epoprostenol, and beraprost (an oral prostacyclin analog that is only available
in Japan), were switched from drug to drug or adopted in combination so as to
achieve these predetermined therapeutic goals once a month. We
performed Cox’s proportional hazard analysis for survival measured from the
date of the diagnosis of PH using propensity score (PS) methods. PS for
CoTpy was estimated from a variety of factors, including sex, age at diagnosis
of PH and CTD, causes for PH, and complicated CTD, using logistic
regression.
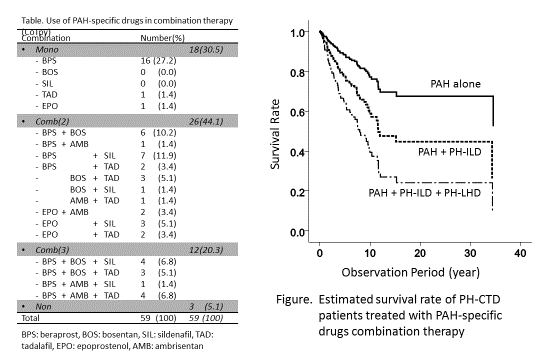
Results: Fifty-nine patients were
treated under our CoTpy strategy. The PAH-specific medications in this
group at the last observation are shown in table 1. Multivariative study
demonstrated that CoTpy significantly reduced the risk for death (HR 0.324, 95%CI:
0.163-0.610) in PH-CTD. Estimated survival curves of patients with PH-CTD
under CoTpy are shown in Figure 1. Thus, coexistence of PH-ILD and PAH
significantly increased the risk for death (HR 1.88, 95%CI: 1.08-3.26) compared
with PAH alone. Moreover, coexistence of PH-ILD and PH-LHD in addition to
PAH increased the risk for death (HR 5.11, 95%CI: 0.822-24.62) compared with
PAH alone.
Conclusion: The results demonstrate
that combination therapeutic strategy using PAH-specific drugs markedly
improved survival of patients with PH-CTD. Moreover, the data indicate
that appropriate management of PH-ILD and/or PH-LHD is important for improving
survival of PH-CTD patients treated with PAH-specific drugs combination
therapy.
To cite this abstract in AMA style:
Tanaka S, Matsueda Y, Ogawa E, Okada J, Hirohata S. Influences of Various Factors on Survival of Patients Treated with Pulmonary Arterial Hypertension-Specific Drugs Combination Therapy in Patients with Connective Tissue Diseases [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/influences-of-various-factors-on-survival-of-patients-treated-with-pulmonary-arterial-hypertension-specific-drugs-combination-therapy-in-patients-with-connective-tissue-diseases/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/influences-of-various-factors-on-survival-of-patients-treated-with-pulmonary-arterial-hypertension-specific-drugs-combination-therapy-in-patients-with-connective-tissue-diseases/